An article written by Dr Edward Leatham, Consultant Cardiologist © 2025 E.Leatham
For busy people, or to tune in when on the move, Google Notebook AI audio podcast and an explainer slide show are available for this story beneath.
Tags: VAT, Metabolic Health, sdLDL CHD, search website using Tags to find related stories.
Two main paths to heart disease
There are broadly two routes that lead to cholesterol build-up in arteries:
- Metabolic or insulin-driven:
Common in people with raised waist size, especially if fasting blood shows high triglycerides, low HDL, or if there is fatty liver disease where the liver overproduces VLDL due to insulin resistance and excess visceral fat.
The result is a rise in sd-LDL — cholesterol-rich particles that contribute to LDL particle number and may not be as cleared by liver LDLR. - LDL-Receptor-driven (often genetic):
Seen in people with inherited conditions like familial hypercholesterolaemia or high PCSK9 levels, where the liver’s LDL receptors don’t clear LDL efficiently.
These patients tend to have larger LDL particles with a high overall particle number.
Many people have a mix of both, especially as they age or gain weight as VAT can also lead to raises PCSK9 activity. That is, in part, why one person can have a “normal” cholesterol reading but still develop heart disease, while another with higher numbers stays healthy.
A new look at cholesterol, insulin, and belly fat
For years, doctors have talked about “good” and “bad” cholesterol. But research now shows the real story is more complicated. Cholesterol itself is essential for life — it’s part of every cell membrane and a building block for hormones and vitamin D.
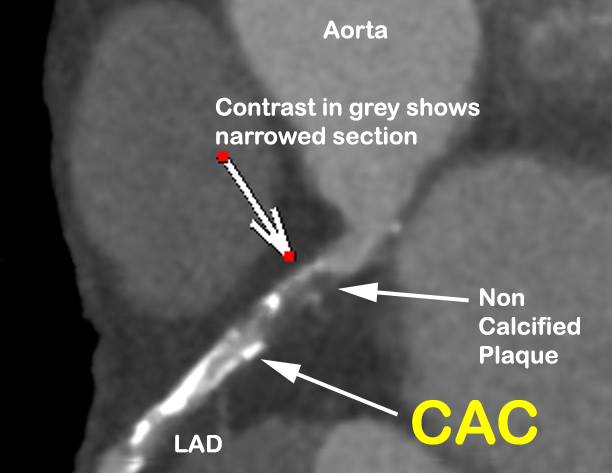
The real trouble starts when too many cholesterol-carrying particles circulate in the blood for too long. These particles, called apoB-containing lipoproteins, can slip through the artery wall, get trapped, and trigger inflammation. Over time, that becomes atherosclerosis — the process that narrows and stiffens arteries.
Where Your LDL Cholesterol Comes From
 FIGURE 1. Metabolism of LDL. Dietary fat is degraded and then absorbed by intestinal cells for the assembly of chylomicron (CM), which is hydrolyzed by lipoprotein lipase (LPL) in circulation to produce chylomicron remnant (CMR). In the liver, apolipoprotein B (ApoB) 100 is critical for the generation of very low-density lipoprotein (VLDL). In blood, plasma VLDL is converted to intermediate low-density lipoprotein (IDL) and low-density lipoprotein (LDL) via hydrolysis of triglycerides (TGs) by LPL and hepatic lipase (HL). Of note, cholesteryl ester transfer protein (CETP) mediates the exchange of cholesterol ester (CE) and TG between high density lipoprotein (HDL) and Apo B-containing lipoprotein, leading to the production of small dense LDL (sdLDL) and small dense HDL (sdHDL), which are atherogenic factors. CMR, IDL, LDL, and sdLDL particles can be cleared by liver through LDL receptor (LDLR), LDLR-related protein 1 (LRP1), heparan sulfate proteoglycan (HSPG), and other potentially unknown receptors. MTP: microsomal triglyceride transfer protein.
FIGURE 1. Metabolism of LDL. Dietary fat is degraded and then absorbed by intestinal cells for the assembly of chylomicron (CM), which is hydrolyzed by lipoprotein lipase (LPL) in circulation to produce chylomicron remnant (CMR). In the liver, apolipoprotein B (ApoB) 100 is critical for the generation of very low-density lipoprotein (VLDL). In blood, plasma VLDL is converted to intermediate low-density lipoprotein (IDL) and low-density lipoprotein (LDL) via hydrolysis of triglycerides (TGs) by LPL and hepatic lipase (HL). Of note, cholesteryl ester transfer protein (CETP) mediates the exchange of cholesterol ester (CE) and TG between high density lipoprotein (HDL) and Apo B-containing lipoprotein, leading to the production of small dense LDL (sdLDL) and small dense HDL (sdHDL), which are atherogenic factors. CMR, IDL, LDL, and sdLDL particles can be cleared by liver through LDL receptor (LDLR), LDLR-related protein 1 (LRP1), heparan sulfate proteoglycan (HSPG), and other potentially unknown receptors. MTP: microsomal triglyceride transfer protein.
Acknowledgement
Figure and explanation from: Qiao Y-N, Zou Y-L, and Guo S-D (2022). Low-density lipoprotein particles in atherosclerosis. Frontiers in Physiology, 13:931931. https://doi.org/10.3389/fphys.2022.931931
© 2022 Qiao, Zou and Guo. This figure is used and modified under the terms of the Creative Commons Attribution License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Whereas the majority of dietary saturated fat bypasses the circulation and is excreted in bile salts, most cholesterol circulating in the blood within LDL is either synthesised by the liver cells or derived from larger particles called VLDL (very low-density lipoproteins) that the liver produces when it has too much fat to export.
Here’s the chain reaction:
- The liver makes VLDL to carry triglycerides (fat) into the bloodstream.
- Enzymes gradually remove triglycerides from VLDL, turning them into smaller particles — first intermediate-density lipoprotein (IDL), then sdLDL.
- These sdLDL particles hang around in the blood because they don’t bind well to the liver’s LDLR clearance receptors.
- The longer they circulate, the more likely they are to become oxidised and trigger plaque formation.
So what causes the liver to churn out excess VLDL in the first place?
That’s where visceral fat and insulin enter the story.
How belly fat and insulin fit into the story
When we eat more calories than we use — especially carbohydrates in people who are carbohydrate-sensitive — the body releases more insulin, a storage hormone.
Insulin tells fat cells to store energy, and the visceral fat around our organs (VAT) is particularly sensitive to this signal.
Over time, high insulin levels drive more triglycerides (fats) into the bloodstream in large “ships” called VLDL particles. As these VLDL particles drop off their cargo to tissues, they shrink into smaller, denser forms of LDL — often called small dense LDL (sd-LDL).
These smaller LDL particles stay in circulation longer and more easily enter the artery wall, where they can trigger inflammation and plaque build-up.
That’s why people with raised triglycerides and low HDL-cholesterol — a common pattern in insulin resistance — are often carrying more of these atherogenic sd-LDL particles, even if their “total cholesterol” looks normal.
The role of the Continuous Glucose Monitor (CGM)
A CGM provides a live feed of your blood glucose throughout the day. For people with a carbohydrate-sensitive phenotype, it’s an invaluable feedback tool.
- It shows how your body responds to different meals, particularly processed foods with added sugars.
- Repeated glucose spikes over 7.8 mmol/L after sugar or carb-heavy meals promote oxidative stress and inflammation.
- Adjusting food choices to flatten these spikes often lowers HbA1c and reflects better metabolic control.
However, research suggests that while these changes improve glucose profiles, they may not drastically reduce overall insulin exposure unless total calorie intake also drops. In short, low-carb diets help most when combined with calorie reduction or increased activity.
The CGM also shows when your insulin levels are low — the best time for exercise if your goal is to burn visceral fat, since fat burning is blocked when insulin is high.
Tracking the early warning signs
Modern cardiology no longer focuses just on LDL-cholesterol.
A comprehensive metabolic picture includes:
- Fasting lipids: rising triglycerides, falling HDL, and higher non-HDL cholesterol suggest more sd-LDL activity.
- Apo B measurement, to assess the number of circulating LDL particles not just total LDL.
- Waist-to-height ratio: a value over 0.5 signals excess visceral fat.
- Liver function tests: rising ALT >25 u/l especially if AST over 32 u/l can indicate fatty liver disease, another clue to VAT excess.
- Low-dose CT scans: used to measure VAT directly and detect early plaque.
- Raised CT Fat Attenuation Index (FAI): highlights coronary inflammation before symptoms appear.
If inflammation remains high after controlling LDL, blood pressure, and insulin resistance, cardiologists sometimes use anti-inflammatory drugs like colchicine — but only after all modifiable risks are addressed.
So, does a statin help?
Yes — statins work mainly by increasing the number of LDL receptors in the liver, which clear LDL particles from circulation.
They lower total LDL effectively, but because sd-LDL binds poorly to these receptors, it isn’t cleared as efficiently. That’s why some people still develop plaque despite having “good” cholesterol numbers.
The key is to address the root metabolic cause — visceral fat and insulin excess — alongside statin therapy.
Putting it all together
Heart disease prevention now goes beyond lowering cholesterol.
It’s about identifying the metabolic phenotype behind the cholesterol:
- Is your LDL high because your liver makes too many particles (from insulin and VAT)?
- Or because your body clears them too slowly (genetic LDL receptor problem)?
- Or both?
Understanding this helps doctors target the right therapy — whether that’s a statin, PCSK9 inhibitor, VAT reduction programme, or GLP-1 therapy.
For many people, the first and most effective steps remain:
- Reducing total calories (especially refined carbs and alcohol)
- Increasing resistance and aerobic exercise
- Tracking waist size and fasting lipids
- Using a CGM for feedback and motivation
The bottom line
Small dense LDL is not a separate disease — it’s a sign that your metabolism is overloaded and your visceral fat stores are driving insulin resistance.
By tackling the root causes — caloric excess, VAT accumulation, and inflammation — you not only reduce sd-LDL but also improve every other aspect of cardiovascular health.
Technical papers: located in Dr Leatham’s “VAT Trap” Digital Companion and Resources
- Why So Many PCSK9 Mutations Exist — Evolution, Immunity, and Trade-Offs
- Cholesterol, LDL, Apo B and sdLDL targets a guide for cardiologists and their patients
- Bradford Hill’s Criteria for Causation Applied to LDL Cholesterol and Coronary Heart Disease
- A Bradford Hill Appraisal of Raised Visceral Adipose Tissue and Coronary Heart Disease:
Related posts
- UK Cholesterol, Apo B, LDL-C Targets
- Cholesterol, LDL, and what we learnt from PCSK9 mutations in familial hypercholesterolaemia
- So what does determine your LDL (‘bad’) Cholesterol?
- LDL: the lower the better
- How to Lose Visceral Adipose Tissue (VAT) and Improve Metabolic Health: A Guide to Sustainable Weight Loss
- Visceral Fat, Mitochondria, and the Energy Trap: Why We Store Fat Where We Shouldn’t
- Why everyone is talking about VAT

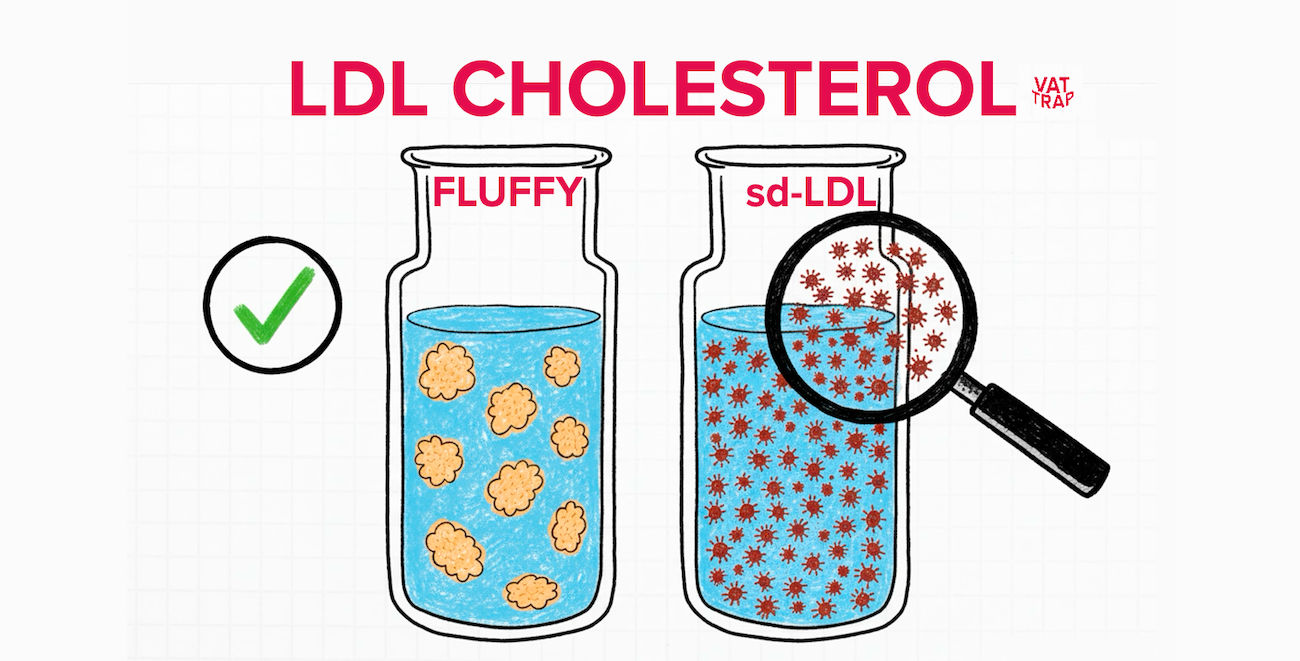
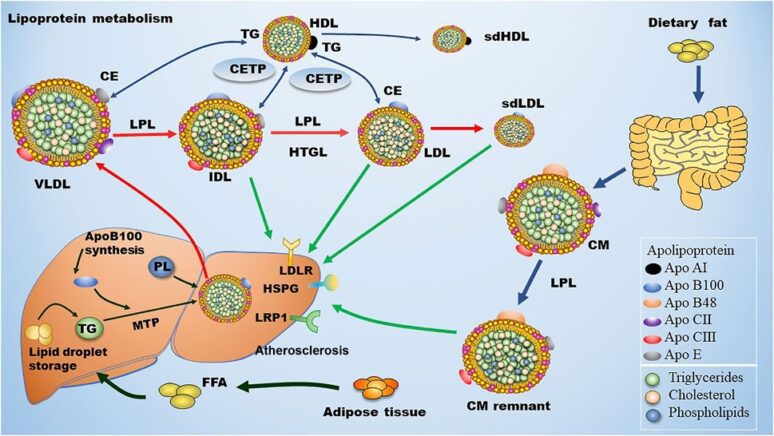 FIGURE 1. Metabolism of LDL. Dietary fat is degraded and then absorbed by intestinal cells for the assembly of chylomicron (CM), which is hydrolyzed by lipoprotein lipase (LPL) in circulation to produce chylomicron remnant (CMR). In the liver, apolipoprotein B (ApoB) 100 is critical for the generation of very low-density lipoprotein (VLDL). In blood, plasma VLDL is converted to intermediate low-density lipoprotein (IDL) and low-density lipoprotein (LDL) via hydrolysis of triglycerides (TGs) by LPL and hepatic lipase (HL). Of note, cholesteryl ester transfer protein (CETP) mediates the exchange of cholesterol ester (CE) and TG between high density lipoprotein (HDL) and Apo B-containing lipoprotein, leading to the production of small dense LDL (sdLDL) and small dense HDL (sdHDL), which are atherogenic factors. CMR, IDL, LDL, and sdLDL particles can be cleared by liver through LDL receptor (LDLR), LDLR-related protein 1 (LRP1), heparan sulfate proteoglycan (HSPG), and other potentially unknown receptors. MTP: microsomal triglyceride transfer protein.
FIGURE 1. Metabolism of LDL. Dietary fat is degraded and then absorbed by intestinal cells for the assembly of chylomicron (CM), which is hydrolyzed by lipoprotein lipase (LPL) in circulation to produce chylomicron remnant (CMR). In the liver, apolipoprotein B (ApoB) 100 is critical for the generation of very low-density lipoprotein (VLDL). In blood, plasma VLDL is converted to intermediate low-density lipoprotein (IDL) and low-density lipoprotein (LDL) via hydrolysis of triglycerides (TGs) by LPL and hepatic lipase (HL). Of note, cholesteryl ester transfer protein (CETP) mediates the exchange of cholesterol ester (CE) and TG between high density lipoprotein (HDL) and Apo B-containing lipoprotein, leading to the production of small dense LDL (sdLDL) and small dense HDL (sdHDL), which are atherogenic factors. CMR, IDL, LDL, and sdLDL particles can be cleared by liver through LDL receptor (LDLR), LDLR-related protein 1 (LRP1), heparan sulfate proteoglycan (HSPG), and other potentially unknown receptors. MTP: microsomal triglyceride transfer protein.