An article first written Oct 2025 updated December 2025 by Dr Edward Leatham, Consultant Cardiologist © 2025 E.Leatham
Tags: VAT, Metabolic Health, NH1, search website using Tags to find related stories.
🩺 Who This Blog Is For
This blog is also part of a book chapter designed to be read either on its own or as part of a broader programme. It was designed initially for our patients with coronary artery disease and high inflammation (measured using FAI CT). It soon became clear that the approach had wider applicability and appeal to anyone with a medical condition such as hypertension, AFib, heart failure or non diabetic hyperglycaemia with one or more of the following:
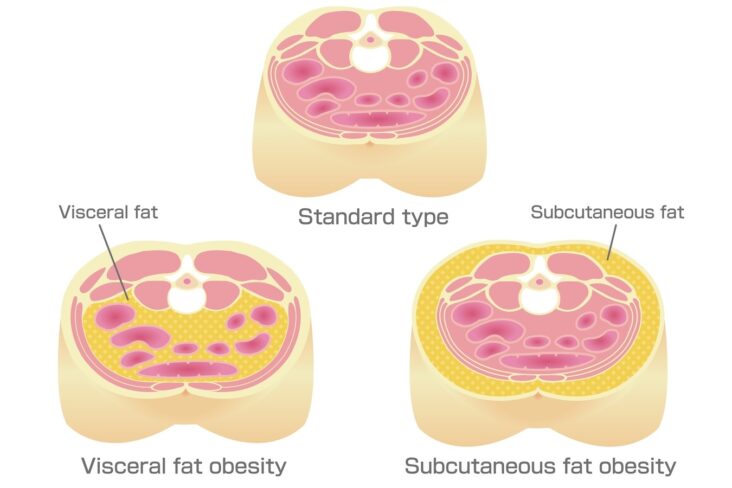
- waist circumference greater than half their height — a strong indicator of elevated VAT
- unhealthy visceral fat on CT or body composition scan
- starting a lifestyle-based approach to reduce VAT, with or without medication
- overweight but not yet eligible or ready for GLP-1 mimetics, who want to measure progress with lifestyle and medical nutrition therapy.
- those taking GLP-1 therapy with a needs to maintain or rebuild skeletal muscle mass to support long-term metabolic health
🔬 How CGM Helps Identify Carbohydrate Sensitivity
Many non-diabetic individuals show significant glucose spikes after carbohydrate intake, especially relevant to those with high VAT, where the combination of natural insulin response to multiple high glucose spikes each day, alongside VAT-induced insulin resistance, sets up a positive feedback loop that promotes further adipose storage.
Continuous Glucose Monitoring (CGM) can reveal this hidden sensitivity.
As part of our Carbohydrate Resilience (CarbR) test, patients wear a CGM for 10–14 days while logging their meals. This allows classification into one of three Glucotypes:
| Glucotype | Response to Carbohydrates |
|---|
| GT1 | can consume high-glycaemic foods without any spikes |
| GT2 | Spikes only after high-glycaemic foods (most common over age 40) |
| GT3 | Spikes even after low-glycaemic foods like oats |
In patients with GT2 or GT3, we diagnose a Carbohydrate-Sensitive Phenotype (CSP) — an innate (probably largely inherited) tendency to spike blood glucose after carbs, carefully labelled to explain the concept and consequences that resemble how patients and society deal with lactose or gluten sensitivity (“a small portion of pasta please as I have CSP”). It helps to Identify CSP in a no-blame way to preface recommendations for adapting some longterm dietary restrictions.
We score current glucose patterns using a 5-point Current Glucose Profile (CGP) scale, where CGP I is optimal, and CGP V reflects poor control. Many patients with CSP are able to shift to healthier CGP levels simply through education and CGM biofeedback.
💪 Building Skeletal Muscle and Exercise for VAT Reduction
Once we have defined Glucotype and dealt with insulin (which signals fat storage) triggered by carbohydrates and sugars, there is still a need to tackle VAT excess.
It should be made clear at the start that this is not a diet or temporary programme. Lowering and maintaining visceral fat requires a lifestyle and nutrition change longterm to reset the brain-VAT set point. Small incremental, progressive and sustainable steps are required alongside a commitment to long term application. In other words with the exception of GLP-1M injections, do not start any of the vat-lowering methods unless you can envisage still doing it in 3 years time!
A multi- facet approach works best, but any one of these will also be a great start:
1. Resistance Training
- Start with Daily 10–15 min sessions see the Youtube playlist we use
- Use dumbbells, resistance bands, or body weight
- Track limb circumference and body composition

2. Cardiovascular Activity
- 7,000–10,000 steps daily
- HIIT 3–4 times per week: short sprints, bike intervals, hill walks
🚴 Why HIIT Is Especially Effective for VAT Reduction
High-Intensity Interval Training (HIIT) is one of the fastest, most efficient ways to lower visceral fat.
HIIT involves short bursts of maximal effort (sprinting, cycling, etc.) alternated with active recovery. Even short 10–20 min sessions have significant metabolic benefits:
- Increases post-exercise fat burn (EPOC)
- Improves insulin sensitivity
- Mobilises abdominal fat
- Enhances mitochondrial function in muscle
🏃 How to Get Started With HIIT
Beginner options:
- 30 sec fast walk / 60 sec normal pace × 6 rounds
- Stationary bike: 15 sec sprint / 45 sec easy × 8 rounds
- Circuit: squats, climbers, jumping jacks, lunges (30 sec on / 30 sec rest)
Aim for 2–4 sessions per week. Combine with resistance training for full-body effect and superior VAT reduction.
HIIT is especially effective for VAT reduction even with short time investment.
Skeletal muscle is your metabolic powerhouse. It’s the primary site for glucose disposal and fat burning. From age 30, we lose muscle mass unless we actively train — which accelerates VAT accumulation.
During weight loss, especially with GLP-1 mimetics, preserving or building muscle is essential for maintaining glucose control and avoiding rebound fat gain.
🧠 Why Building Muscle Is Your Best Defence
Skeletal muscle isn’t just for movement — it is your glucose sink. It burns energy, supports metabolism, and prevents excess insulin release. To reduce VAT, you must:
- Preserve or increase muscle
- Avoid long periods of inactivity
- Focus on strength as much as fat loss
This is why even patients using GLP-1 mimetics must prioritise resistance training — to avoid losing lean mass alongside fat.
🍗 Why Prioritising Protein Works Metabolically
One of the most overlooked contributors to rising VAT is loss of skeletal muscle, which houses the majority of the body’s mitochondria — the engines responsible for burning glucose.
From around age 30, we begin to lose muscle mass (sarcopenia), in part due to anabolic resistance. As we age, our muscles become less responsive to small amounts of protein.
If we don’t eat enough — especially if we sit too much — the body breaks down our own muscle to get the amino acids it needs. This leads to muscle loss, weakness, slower metabolism, and poorer health.
Eating enough protein and doing resistance training protects muscle as we age.
Why losing muscle impacts metabolic health
Less muscle means fewer glucose receptors and slower glucose clearance. This leads to:
- More glucose remaining in circulation after meals
- More insulin release to compensate
- More energy stored as fat — initially subcutaneous, but eventually as visceral fat
As VAT accumulates, it drives inflammation, insulin resistance, and metabolic dysfunction — creating a vicious cycle.
One of the most powerful strategies in reducing visceral fat is not just eating less — but eating differently.
Specifically, replacing some of your daily carbohydrate and fat intake with protein provides multiple benefits, especially if you have high VAT and/or a carbohydrate-sensitive phenotype (CSP).
🔬 Why Protein Is Different From Carbs and Fat
- Fat and carbohydrates are easily stored in the body when eaten in excess — especially when insulin is elevated.
- Protein, by contrast, cannot be easily stored. The body lacks a “protein bank.”
Any surplus amino acids must be either:
- Used immediately for tissue repair (e.g. muscle rebuilding), or
- Deaminated — a process that removes the nitrogen-containing amino group, leaving behind a carbon skeleton (like acetyl-CoA) that can be used for energy.
🔥 Protein Has a Built-in Calorie Penalty
This deamination process costs energy, meaning your body burns calories to process excess protein. As a result:
- Fewer net calories are stored from protein than from carbs or fat
- Thermic effect of protein is significantly higher (20–30%) than carbs (5–10%) or fat (0–3%)
- Protein increases dietary-induced thermogenesis, raising your metabolic rate after eating
This is one of the reasons high-protein diets — such as Atkins — often result in fat loss even without strict calorie counting.
🛡️ Double Benefit: Supports Muscle, Reduces Storage
For those engaging in resistance training, higher protein intake also helps build and maintain muscle, which is essential for long-term VAT reduction and metabolic health.
Even in those not yet strength training, increasing protein can:
- Boost satiety (you feel fuller, longer)
- Reduce insulin spikes compared to high-carb meals
- Minimise fat storage due to the metabolic inefficiency of converting protein to energy
✅ Summary: Why It Works
| Macronutrient | Easy to Store? | Triggers Insulin? | Thermic Effect | Can Build Muscle? | Caloric Efficiency |
|---|
| Carbs | Yes | Yes | Low | No | High (efficient) |
| Fat | Yes | No | Very Low | No | High (efficient) |
| Protein | No | Minimal | High | Yes | Low (inefficient) |
🛠️ Your VAT Reduction Toolkit
To effectively reduce VAT without medication, we combine four key principles:
| Strategy | Why It Works |
|---|
| Build muscle | Increases mitochondrial mass and glucose disposal capacity |
| Restrict calories | Creates energy deficit to mobilise stored fat |
| Avoid glucose spikes | Especially important in CSP, to reduce insulin and fat storage |
| Increase protein intake | Supports muscle repair and reduces hunger |
Let’s look at the tools you can use at home to track your progress.
📏 Waist Circumference
Your most powerful, low-cost indicator of VAT change.
- Use a flexible tape measure
- Measure just above the belly button each morning
- Keep the tape level and snug but not tight
- Waist should be < half your height
🍽️ Food Tracking Apps
Apps such as Dr Shape, MyFitnessPal, or MacroFactor help reduce guesswork and reveal hidden patterns:
- Set calorie and macronutrient targets (especially protein)
- Photograph meals for real-time feedback (in some apps)
- Identify under-eating, snacking, or excessive carbohydrate intake
Most patients are surprised to learn they are:
- Eating too little protein
- Eating more carbs than they realise
- Eating at irregular times, which spikes insulin
📊 CGM or Glucose Monitoring
We recommend everyone use a CGM for 2 weeks — or a finger-prick monitor if unavailable — to track glucose excursions.
- Aim to avoid spikes >7.8 mmol/L after meals
- Observe how specific foods affect you
- Tailor your intake accordingly
If your glucose spikes after bread, rice, beer, or fruit juice — and you have a high waist:height ratio — it’s highly likely you have CSP, and would benefit from long-term reduction in high-glycaemic carbohydrates.
🧬 Adjustments for CSP
Patients with Glucotype 2 or 3 (CSP) often benefit from:
- Lower carb targets
- Higher protein and fibre
- Meal sequencing (fat and fibre before carbs)
This flattens glucose curves, reduces insulin, and supports VAT loss.
⏰ Time-Restricted Eating (TRE)
In CSP and non-CSP patients alike, when you eat also matters.
Time-Restricted Eating (TRE) involves eating within a daily window, commonly:
- 16:8 (16-hour fast, 8-hour eating)
- 14:10 (easier to start)
- 12:12 (gentle beginning)
Benefits of TRE:
- Reduces insulin exposure
- Promotes fat oxidation
- Improves appetite regulation
- Supports circadian rhythm
Start with 12:12, then extend as tolerated. Fasting is optional, but particularly helpful in CSP where fewer glucose peaks mean better VAT control.
📅 Tracking Your Progress
Track these weekly:
- Weight
- Waist circumference
- Muscle mass (if using body composition scales)
Track these monthly:
Reassess with your clinical team after 12 weeks, and consider a CT scan at 6 months to confirm VAT reduction if needed.
At SCVC we developed a 12 month tracker booklet called N-of-1 that anyone can purchase on Amazon or via the Cardiometabolic toolkit

🧠 Optional Add-Ons
- AI dietitian support (every 2 weeks via app or platform)
- CarbR Test for those without access to CGMs
- Time-restricted eating coaching
- GLP-1 mimetics if VAT remains high after 6 months of structured lifestyle change
🔄 Summary Table: Non-Medication VAT Reduction
| Goal | Tool or Strategy |
|---|
| Reduce visceral fat | Waist tape, Renpho, body composition tracking |
| Preserve/build lean mass | Resistance training, high protein intake |
| Create calorie deficit | Food app (Dr Shape, MacroFactor, MyFitnessPal) |
| Control glucose/insulin | CGM, CarbR test, food sequencing |
| Adjust macros for CSP | Lower carbs, higher protein/fibre, avoid snacking |
| Enhance metabolism | TRE, HIIT, step count, regular movement |
| Review progress | Clinical review at 12 weeks, optional CT at 6 months |
🎯 Final Message
You can reduce visceral fat without medication — but it requires consistency, insight, and personalised feedback. This is not a one-size-fits-all programme. It’s a guided experiment, and you are the subject.
By tracking your inputs and your body’s responses, you’ll discover your own formula for health.
Related posts
- Cardiometabolic toolkit
- How to Reduce Visceral Fat Without Medication
- Why Protein Matters More Than Ever as We Age
- How to Lose Visceral Adipose Tissue (VAT) and Improve Metabolic Health: A Guide to Sustainable Weight Loss
- Why everyone is talking about VAT
- Examples of CT VAT scans and normal ranges for VATI
- Visceral Fat, Mitochondria, and the Energy Trap: Why We Store Fat Where We Shouldn’t
- Carbohydrate Sensitive Phenotype (CSP): Precursor of the Metabolic Syndrome?
- Exercise and Digital Tools Should Be the First Line in Reducing Visceral Fat in Cardiac Patients
- Cardiologists and a New Enemy: Evolving Tools of the Trade
- Carbohydrate Sensitive Phenotype (CSP): Precursor of the Metabolic Syndrome?
- Metabolic Health Assessment
- Biofeedback: CGM metrics improve after just 4 weeks of dietary intervention
- Lets compare continuous glucose monitor (CGM) results