An article written by Dr Edward Leatham, Consultant Cardiologist © 2025 E.Leatham
Recent findings from the SURMOUNT-4 programme once again demonstrate a predictable pattern: when patients are treated with high-dose GLP-1/GIP therapy for a fixed period and then withdrawn abruptly, much of the weight loss — and most of the metabolic benefit — is lost within 12-24 months. Waist circumference rises, insulin resistance returns, and cardiometabolic risk drifts back towards baseline.¹
The pattern observed in SURMOUNT-4 and STEP-1 is no longer confined to individual trials. It has now been confirmed at population level. A 2026 systematic review and meta-analysis published in the BMJ examined weight and metabolic outcomes after cessation of pharmacological weight-management therapies across multiple drug classes and trial designs.² The findings were consistent and striking:
- Weight regain is the norm, not the exception, after medication withdrawal
- The majority of lost weight is regained within months
- Metabolic improvements regress in parallel
- No drug class demonstrated durable benefit once treatment stopped without accompanying behavioural and physiological change
Importantly, the authors conclude that this pattern reflects biological defence of body weight and metabolism, rather than patient non-adherence.
These findings reinforce the central message of this article:
withdrawal without system change predictably fails.
They also support the need for longer term cardiology-led prevention programmes that prioritise:
- visceral fat reduction,
- muscle function and metabolic protection,
- behavioural feedback loops,
- and gradual medication tapering rather than abrupt cessation.
The Core Error in Withdrawal-Based Models
Most GLP-1 trials follow the same structure:
- Escalate medication aggressively
- Achieve rapid weight loss
- Withdraw treatment
- Observe relapse
This assumes metabolic health behaves like a switch. Biology does not.
Without sustained changes in:
- visceral adipose tissue (VAT),
- skeletal muscle function,
- dietary protein intake,
- glycaemic behaviour,
- and behavioural reinforcement,
the body simply re-establishes its prior metabolic set point.
When medication stops but nothing underneath has changed, physiology defaults backwards.
As cardiologists managing hypertension and dyslipidaemia, we were never under any illusion that a powerful drug would confer lasting benefit once withdrawn. Blood pressure- and lipid-lowering therapies generally need to be continued long term, often for life. We also recognise that many patients are understandably reluctant to commit to a weekly injection indefinitely. From the outset, therefore, our goal was to improve metabolic health through sustainable lifestyle and nutritional change, knowing that short-lived diets or sporadic gym attendance rarely succeed.
Careful analysis of the GLP-1 cardiovascular outcome trials led us to conclude that much of their benefit is mediated through reduction in visceral adipose tissue (VAT) — a key driver of insulin resistance and small dense LDL production. This insight shaped our clinic model. By prioritising VAT reduction, healthier eating, and skeletal muscle preservation, we create a strong physiological foundation. GLP-1 therapy can then be added at low dose to reduce food noise and interrupt the VAT–insulin “doom loop”, making metabolic recovery achievable with lower doses and a realistic prospect of intermittent or permanent withdrawal, provided resistance training and dietary changes are maintained.
Our Programme Starts From a Different Premise
SCVC’s cardiometabolic programme is not designed to “come off” a drug.
It is designed to change the system the drug is acting on.
A significant proportion of patients referred for our programme are in the normal BMI with high body fat category – often called “skinny fat,” medically known as Normal Weight Obesity (NWO) or Metabolically Obese Normal Weight (MONW), diagnosis suspected by a waist to height ratio >0.5, often confirmed by low dose VAT-CT. All patients are introduced to the programme as:
- gradual layering of lifestyle and behavioural interventions
- N-of-1 experimentation, rather than rigid protocols
- supported where needed by micro-dose GLP-1 therapy, not maximal escalation in most cases.
Medication supports the process — it does not define it.
The aim is to build metabolic resilience, so that medication tapering represents a gentle slope, not a metabolic cliff.
Entry Criteria: A Cardiometabolic Clinic, Not Weight Management
It is important to be explicit:
this is not a weight-loss clinic.
Patients entering our 8 month programme typically have one or more of the following:
- coronary heart disease,
- raised coronary inflammation on CT (FAI),
- hypertension,
- atrial fibrillation,
- raised cardiometabolic risk driven by raised visceral adipose tissue (VAT), with or without elevated BMI.
Our objective is cardiometabolic risk reduction:
- lowering VAT,
- preserving or rebuilding skeletal muscle,
- improving insulin sensitivity,
- reducing long-term cardiovascular risk.
Weight loss is a secondary consequence, not the therapeutic target.
The SCVC Four-Tier Feedback Model: How We Prevent Misinterpretation
To avoid conflicting signals and patient anxiety, we use a hierarchical feedback system, described in detail in our earlier clinician paper (Figure 1: The SCVC Four-Tier Feedback Model).
This framework ranks signals by physiological importance, not convenience.

Figure 1: the four tiers of feedback used to reinforce progress towards metabolically healthy VAT.
Nutrition Comes First: Dr Shape as Food Analysis and Coach Bot
All patients are provided with Dr Shape, an AI-enabled food analysis and coach bot.
Patients photograph meals and receive:
- real-time macronutrient analysis,
- tracking against clinician-set targets for protein, fibre, and carbohydrate,
- daily prompts that reinforce learning and consistency.
Dr Shape functions as daily support between clinic visits, at very low cost, helping patients understand:
- what adequate protein intake actually looks like,
- how fibre and fats modify glycaemic response,
- which carbohydrate patterns destabilise appetite and glucose.
The goal is education and habit formation, not lifelong tracking.
Strength Is the Primary Muscle Signal (Tier 2)
As outlined in the clinician paper Functional Strength Overrides Bioimpedance, we track muscle function, not estimated mass.
We prioritise:
- 30-second sit-to-stand testing (arms crossed),
- handgrip strength, in clinic or at home.
Strength reflects mitochondrial density, neuromuscular efficiency, and metabolic protection — particularly in older adults.
Rule: If waist circumference is falling and strength is rising, muscle health is improving — regardless of what the scales report.
Our strength test is designed for anyone to use at home see https://link.scvc.co.uk/testyourstrength
Where bioimpedance scales Fit In — and Where Does Not (Tier 4)
Most of our patients are now supplied with bioimpedance scales, with data reviewed by our team. There is a significant psychological benefit from medical team oversight that helps keep patients on track, however we all need to remember the hierarchy:
- GLP-1 drugs reduce insulin, glycogen, inflammation, and body water,
- bioimpedance therefore can underestimate lean mass during metabolic improvement.
This is artefact, not sarcopenia.
Accordingly:
- body composition data should not be interpreted in isolation,
- they are used for engagement, reassurance, and trend awareness only.
If the body composition scales suggests falling “muscle mass” while strength and resistance load are increasing, clinicians would suspect measurement limitation, not biological loss.
Clinical oversight prevents inappropriate responses.
An example: three panels, one story: why hierarchy matters in metabolic tracking
These three panels show what can happen when different feedback tools are interpreted without a hierarchy.

Bioimpedance data shown are representative examples used for educational discussion. Similar limitations apply to all consumer bioimpedance devices, particularly during pharmacologically induced changes in hydration and metabolism.
Left panel – Waist circumference (Tier 1 signal)
Between August 2025 and January 2026, waist circumference falls steadily from 103.3 cm to 98.7 cm. This is a direct, low-noise surrogate of visceral adipose tissue (VAT) and indicates sustained reduction in the primary driver of cardiometabolic risk.
Middle panel – Bioimpedance “skeletal muscle mass”
Over the same period, the bioimpedance scale suggests skeletal muscle initially rises, then falls from December onwards. Taken at face value, this would imply emerging sarcopenia during treatment with weekly tirzepatide 5 mg.
Right panel – Bioimpedance “body fat mass”
The same scale simultaneously reports an increase in body fat mass, directly contradicting the falling waist measurement.
Now add the missing context. During December, daily 10-minute resistance training was performed consistently, with strength clearly improving: dumbbells increased from 4 kg to 7 kg. Functional capacity rose, not fell.
Putting the hierarchy back in place resolves the paradox:
- Tier 1 (waist/VAT) is falling → visceral fat is reducing
- Tier 2 (strength/function) is improving → muscle health is improving
- Therefore, the Tier 4 bioimpedance outputs (muscle ↓, fat ↑) must be measurement artefact, not physiology
GLP-1 therapy alters hydration, glycogen, inflammation, and water compartments. Bioimpedance algorithms misclassify these changes as “muscle loss” and “fat gain”.
This figure illustrates the core lesson:
when simple, high-signal measures (waist and strength) improve, conflicting scale data should be de-weighted, not acted upon.
Only by combining metrics within a tiered feedback framework can apparently contradictory results be interpreted safely and correctly.
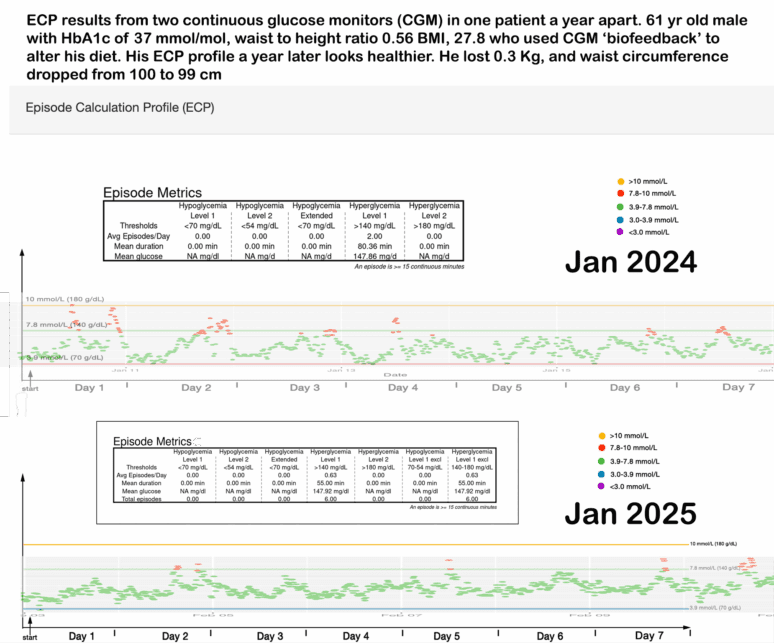
CGM: Behavioural Feedback, Not Judgement (Tier 3)

The continuous glucose monitor (CGM) shows real time glucose, with healthy values (under 7.8 mmol/L/ 110 mg/dL), unhealthy values over 7.8 and 10 mmol/L in red illustrated here.
Patients see their physiology responding within minutes of intake of high glycaemic foods. This type of feedback transforms behaviour — far faster than any traditional diet advice sheet.
In patients with a carbohydrate-sensitive phenotype, we therefore use continuous glucose monitoring (CGM) to provide powerful behavioural feedback.
CGM helps patients:
- identify foods that provoke glucose excursions,
- adjust choices during GLP-1 tapering,
- reinforce decisions that support VAT reduction.
CGM is a training tool, not a pass/fail test.
Removing Negative Levers
We deliberately avoid:
- pushing our patients into potentially costly gym memberships, that may be unrealistic to use in the long term.
- complex meal plans,
- unrealistic exercise expectations.
Instead, we promote low-friction habits that compound over time.
Home-Based Resistance Training
Patients are encouraged to perform:
- 10–30 minutes,
- at home,
- using bodyweight, bands, or light dumbbells.
Consistency matters more than intensity. Strength improves faster than most expect.
N-of-1 Experiments: Personal Physiology Beats Population Averages
Each week, patients using GLP-1 support choose between:
- a small GLP-1 dose adjustment, or
- a lifestyle experiment.
Outcomes are tracked across:
- waist circumference (Tier 1),
- strength tests (Tier 2),
- CGM and dietary behaviour (Tier 3),
- supportive trends only (Tier 4).
RCTs show population averages.
N-of-1 data shows your personalised physiology.
Conclusion
Withdrawal trials show what happens when medication stops and nothing else changes.
Our cardiometabolic programme changes:
- visceral fat,
- muscle function,
- glucose behaviour,
- nutrition,
- feedback,
- and incentives.
By applying the SCVC Four-Tier Feedback Model, we build metabolic resilience, not transient weight loss.
This is cardiology — not dieting.
References
- Tirzepatide withdrawal and cardiometabolic rebound (SURMOUNT-4).JAMA Internal Medicine.https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2841273
- Weight regain after cessation of medication for weight management: systematic review and meta-analysis.
BMJ 2026;392:e085304. doi:10.1136/bmj-2025-085304 Published 07 January 2026. Open access (CC BY). - Semaglutide withdrawal study (STEP-1 extension).
Diabetes, Obesity and Metabolism. https://pubmed.ncbi.nlm.nih.gov/35441470/
Related posts
- How to Reduce Visceral Fat Without Medication
- Turn the Thermostat Down: How a Cooler Home May Improve Insulin Sensitivity and Reduce VAT
- THE CHOICE: How Cardiologists Operate GLP-1 Mimetics in Practice
- Biofeedback: CGM metrics improve after just 4 weeks of dietary intervention
- What Your Glucose Curve Is Trying to Tell You: Why Continuous Glucose Monitoring Matters Long Before Diabetes
- How to Lose Visceral Adipose Tissue (VAT) and Improve Metabolic Health: A Guide to Sustainable Weight Loss
- Protein, Sarcopenia, and the Pursuit of Healthspan
- Why Protein Matters More Than Ever as We Age