An article written by Dr Edward Leatham, Consultant Cardiologist
Tags: VAT, Metabolic Health, NH1, search website using Tags to find related stories.
In an era when cardiovascular disease remains a leading killer in the UK, the imperative is shifting: we need not only to treat disease when symptoms emerge, but to intercept its metabolic antecedents well before the damage becomes irreversible. At the Surrey Cardiovascular Clinic (SCVC), we are proud to have developed a distinctive set of cardiometabolic services that aim to do just that — to help patients improve their metabolic health, reduce visceral adipose tissue (VAT), and thereby reduce their long-term risk of coronary heart disease, heart failure and other cardiovascular complications.
Having been established to deliver advanced cardiovascular care and prevention, SCVC is now evolving into a specialist centre for both early detection of coronary artery disease and metabolic dysfunction. By combining powerful imaging, deep metabolic phenotyping, and tailored intervention programmes, we seek to offer patients a pathway from risk to resilience.
Below I outline the rationale, methods, and programmes we offer, and the philosophy that underlies them.
The rationale: metabolic dysfunction as a silent driver of cardiovascular disease
Many patients who present with hypertension, atrial fibrillation, or early coronary lesions also harbor subtle—but clinically important—metabolic abnormalities that long predate overt disease. Even in the absence of diagnosable diabetes, dysregulated glucose metabolism (for example, frequent post-prandial glucose spikes), insulin resistance, visceral fat accumulation and subclinical inflammation may accelerate atherosclerosis, promote endothelial dysfunction, and drive ectopic fat deposition (including in the pericardium, liver, pancreas, etc.).
Visceral adipose tissue is metabolically active: in contrast to subcutaneous fat, VAT secretes inflammatory adipokines and free fatty acids into the portal circulation, contributes to insulin resistance and lipotoxicity, and exacerbates systemic metabolic stress. Patients with elevated VAT are at higher risk not only of progression to type 2 diabetes, but also of cardiovascular events, heart failure, and poorer outcomes in multiple organ systems.
In recent years, cardiology has begun to embrace metabolic therapies more aggressively. GLP-1 receptor agonists, for instance, are being used in patients with coronary disease and obesity to achieve weight and VAT reduction, beyond their glycaemic effects. But to apply these therapies effectively, and in a targeted way, we believe the key is to detect patients early—ideally decades before overt disease emerges—and to intervene with precision.
Thus, in our view, an optimal preventative cardiometabolic clinic must offer:
- Early detection of coronary disease activity (beyond stenosis alone)
- Sensitive metabolic phenotyping, even in non-diabetic patients
- Tailored intervention options (diet, exercise, psychological support)
- A scalable escalation path (from lifestyle alone, to pharmacotherapy as needed)
- Close phenotypic feedback (imaging, glycaemic monitoring, body composition)
It is the integration of diagnostics and therapeutics, with continuous feedback loops, that distinguishes SCVC’s approach.
SCVC: a specialist centre for early detection and metabolic care
At SCVC, we are positioned uniquely in Surrey and the South East as a centre of excellence outside a hospital environment, dedicated to cutting-edge cardiovascular prevention and metabolic services.
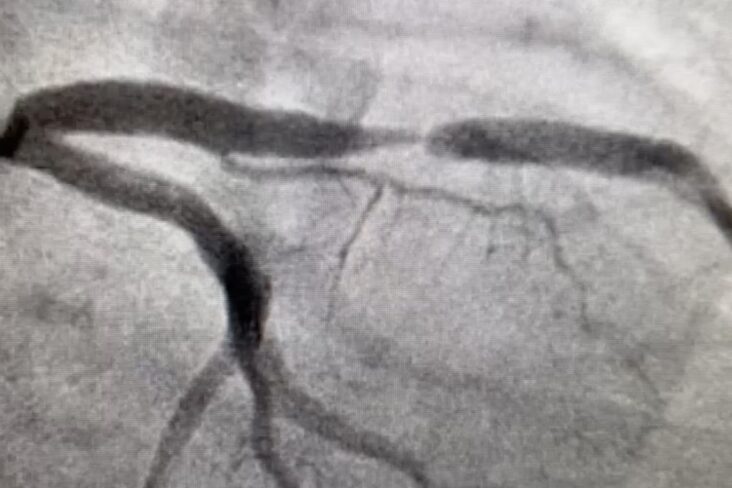
Early detection of coronary disease activity: FAI and CaRi-Heart
Traditional CT angiography and calcium scoring detect structural plaque or calcification. Yet many vascular events originate in segments with non-obstructive disease or in areas of active inflammation, not necessarily those causing high-grade stenosis. To bridge this gap, we have integrated the Caristo / CaRi-Heart platform into our imaging offering. SCVC collaborates with VCL Surrey and Caristo Diagnostics to provide CaRi-Heart assessments with Fat Attenuation Index (FAI) as a biomarker of coronary inflammation. (Caristo.com)
 In the Caristo report above the FAI score is 21 – over the 90th centile – indicating high coronary inflammation with high risk of coronary events within 8 years. We observe that aggressive LDL reduction and optimisation of metabolism lowers the FAI score and improves prognosis.
In the Caristo report above the FAI score is 21 – over the 90th centile – indicating high coronary inflammation with high risk of coronary events within 8 years. We observe that aggressive LDL reduction and optimisation of metabolism lowers the FAI score and improves prognosis.
The FAI (Fat Attenuation Index) measures local perivascular fat attenuation changes on CT imaging, which reflect alterations in the biochemical state of the vascular wall and local inflammation. An abnormal FAI score is associated with markedly higher risk of fatal coronary events and major adverse cardiac events (MACEs). (Caristo.com) Using this AI-derived metric alongside plaque imaging and classical risk factors, CaRi-Heart enables us to stratify patients much more finely and detect early coronary disease activity even when stenoses are minimal. (Caristo.com)
Thus, in patients with risk factors (e.g. hypertension, dyslipidaemia, strong family history), we can deploy a coronary CT scan (a specialised CT protocol) plus FAI analysis to assess both anatomical and inflammatory risk long before clinical symptoms. This allows us to identify patients who might benefit from earlier and more aggressive preventive therapy.
This imaging arm complements our metabolic services by providing a feedback end-point: as metabolic interventions reduce inflammatory burden and visceral adiposity (or slow progression), one might anticipate improvements in FAI or plaque progression—thus closing the loop between metabolism and vascular health.
Metabolic phenotyping: detecting early dysfunction
In parallel, SCVC offers a suite of metabolic tools to detect dysfunction long before conventional metrics (e.g. HbA1c) become abnormal. Because many individuals with “normal” laboratory values already experience glucose excursions, insulin surges, and progressive visceral fat deposition, we believe an aggressive screening and feedback strategy is essential.
Our metabolic services include:
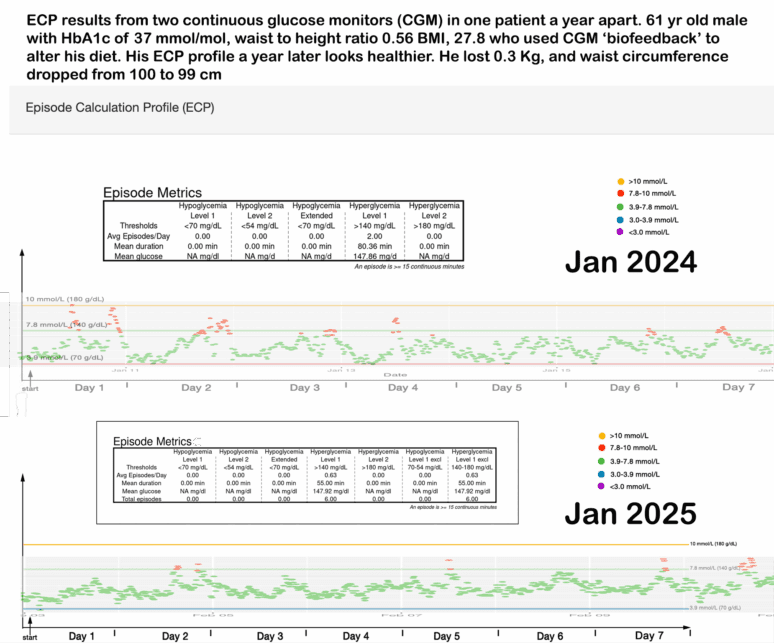
Continuous Glucose Monitoring (CGM)
We deploy CGMs to identify the so-called “carbohydrate sensitivity” phenotype. This allows us to observe post-prandial glucose spikes and excursions in real time, even in non-diabetic individuals. Many patients with apparently normal HbA1c or fasting glucose exhibit repeated glycaemic excursions above thresholds (e.g. >7.8 or >10 mmol/L) that conventional lab tests miss.
These excursions are not benign: each spiking episode stimulates insulin release, promotes oxidative stress and inflammation, and may accelerate atherogenesis. Over time, repeated spikes drive insulin resistance and visceral fat deposition.

By providing CGM feedback, we can guide patients to avoid high glycaemic loads (even from “healthy-seeming” sources like high-fructose fruit), smooth their glucose curves, reduce insulin surges, and slow or reverse metabolic progression.

- Carbohydrate Resilience Test (“CarbR”)
We offer a home-based metabolic challenge to assess how robustly an individual handles a carbohydrate load. This may involve sequential glucose monitoring and controlled carbohydrate challenges to distinguish resilient from sensitive phenotypes. This helps tailor dietary prescription more precisely: low-glycaemic diets for those with sensitivity, more liberal intake for resilient individuals. - Formal Metabolic Health Assessment
In addition to CGM and CarbR, in some cases we dig deeper and perform a full metabolic profile, including lipidomics, insulin, pro-atherogenic proteins (such as Lp(a)), glycaemic indices, inflammatory markers, and other advanced biomarkers. This comprehensive phenotyping helps stratify underlying drivers, beyond what standard panels reveal.
Patients who undergo this combined phenotype mapping often find the results eye-opening: they gain actionable insight into exactly how their diet, sleep, exercise, and stress interact in their individual metabolism.
4. Gene testing

Many of our individual responses to food and micronutrients are determined by our genes, and which polymorphisms we inherit. This fact explains why a detailed gene test to establish predisposition is proving extremely popular.
We offer the Nutrigenomix test to our patients and their families who wish to explore their genetic code, for a more individualised approach to nutrition.
Where sophisticated testing identifies higher risk we have a range of treatments and interventions that are customised to suit each patients needs. These are outline in the next blog.
Related posts
- Intervention programmes: from self-toolkits to nurse-led escalation to GLP-1 support
- Cardiometabolic toolkit
- Visceral Fat, Mitochondria, and the Energy Trap: Why We Store Fat Where We Shouldn’t
- Carbohydrate Sensitive Phenotype (CSP): Precursor of the Metabolic Syndrome?
- Exercise and Digital Tools Should Be the First Line in Reducing Visceral Fat in Cardiac Patients
- Cardiologists and a New Enemy: Evolving Tools of the Trade
- Carbohydrate Sensitive Phenotype (CSP): Precursor of the Metabolic Syndrome?
- Metabolic Health Assessment
- Biofeedback: CGM metrics improve after just 4 weeks of dietary intervention
- Lets compare continuous glucose monitor (CGM) results


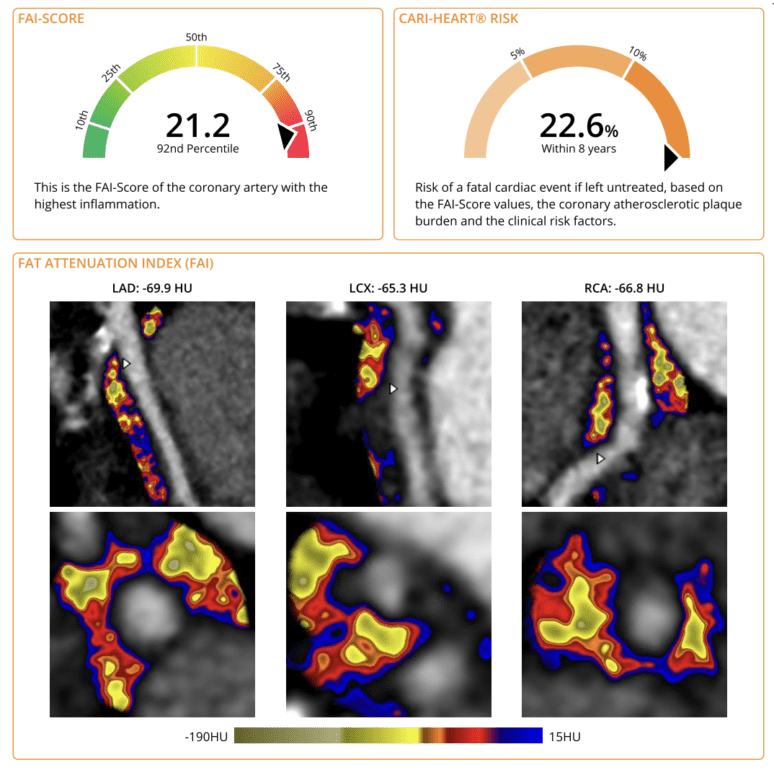 In the Caristo report above the FAI score is 21 – over the 90th centile – indicating high coronary inflammation with high risk of coronary events within 8 years. We observe that aggressive LDL reduction and optimisation of metabolism lowers the FAI score and improves prognosis.
In the Caristo report above the FAI score is 21 – over the 90th centile – indicating high coronary inflammation with high risk of coronary events within 8 years. We observe that aggressive LDL reduction and optimisation of metabolism lowers the FAI score and improves prognosis.