An article written by Dr Edward Leatham, Consultant Cardiologist © 2025 E.Leatham
For busy people, or to tune in when on the move, Google Notebook AI audio podcast and an explainer slide show are available for this story beneath.
Tags: VAT, Metabolic Health, NH1, search website using Tags to find related stories.
Epigenetics and Metabolic Health: How Lifestyle Rewrites Your Genes
We used to think our genes were fixed — a biological script handed down at birth, determining everything from eye colour to heart disease. But modern science has shown that this script can be edited in real time. The field that studies these changes is called epigenetics, and it’s one of the most exciting developments in understanding why some people develop metabolic problems while others stay healthy.
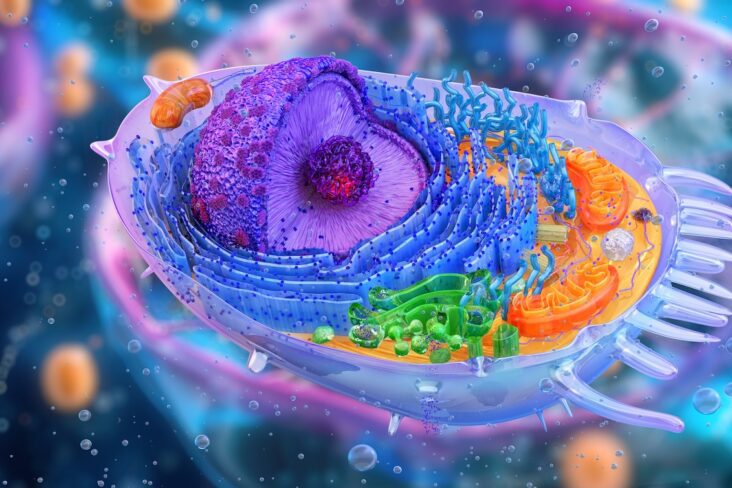
Genes Are the Hardware — Epigenetics Is the Software
Think of your DNA as the hardware in a computer — the physical circuitry that doesn’t change. Epigenetics is the software that tells the system what to do. It controls which genes are switched on or off, when, and how strongly.
These switches are controlled by small chemical tags — such as methyl groups — that attach to DNA or to the histone proteins around which DNA is wrapped. The process doesn’t alter your genetic code but changes how it’s read. In effect, the body can fine-tune its own biology depending on environment, nutrition, and stress.
Twin Studies: Nature’s Perfect Experiment
Identical twins provide one of the clearest demonstrations of epigenetics in action. They start life with the same DNA, yet often end up with very different health profiles.
Researchers have shown that as twins age, their DNA methylation patterns diverge — especially when their diets, activity levels, and stress exposures differ. One twin may stay metabolically healthy, while the other develops excess visceral fat, insulin resistance, or hypertension.
This difference isn’t genetic — it’s epigenetic programming, driven by lifestyle. Our everyday choices literally leave chemical fingerprints on our DNA, changing how our metabolism works.
How Epigenetics Shapes Metabolic Health
Epigenetic regulation affects thousands of genes involved in:
- Glucose handling – how efficiently we store or burn sugar.
- Fat storage – whether energy is parked safely under the skin or viscerally around the organs.
- Inflammation – the low-grade immune activation linked to insulin resistance.
- Mitochondrial function – how well our cells convert fuel to energy.
In short, epigenetics is the molecular bridge between lifestyle and disease. It explains why two people eating the same meal can have very different glucose spikes, and why decades of stress or sleep loss can push one individual towards metabolic syndrome while another remains resilient.
Can We Reverse Epigenetic Damage?
The hopeful news is that epigenetic changes are dynamic — they can often be reversed. Studies show that improvements in diet, physical activity, and sleep can remodel methylation patterns within weeks to months.
For example, regular resistance training and a diet rich in phytonutrients, omega-3 fats, and adequate protein have all been linked to favourable epigenetic profiles — switching on genes that promote fat oxidation, mitochondrial biogenesis, and anti-inflammatory pathways.
This is one reason why people who adopt structured metabolic reset programmes — focusing on visceral fat reduction, stable glucose control, and muscle preservation — often experience such profound health shifts. Their DNA hasn’t changed, but how their body reads it has.
Epigenetics in the VAT Trap
In The VAT Trap, I describe how visceral adipose tissue (VAT) acts as both a marker and a driver of metabolic disease. Epigenetic mechanisms are central to this process. Chronic energy overload, particularly from high-glycaemic carbohydrates, drives insulin and cortisol signals that alter gene expression within adipose tissue and the liver.
Over years, this programming locks the body into a “fat-storing” mode. Yet by interrupting that cycle — through nutrition, sleep, and stress control — we can reset the metabolic code.
Epigenetics reminds us that the body is not a machine doomed by its factory settings. It’s a living, adaptive system — responsive, flexible, and open to reprogramming at any age.
Key Idea
Epigenetics explains why lifestyle change works.
It’s not just willpower or weight loss — it’s the reprogramming of your biology at the level of gene expression. What you eat, how you move, and how you sleep are instructions written directly into your DNA’s operating system.
Technical papers: located in Dr Leatham’s “VAT Trap” Digital Companion and Resources
- Why So Many PCSK9 Mutations Exist — Evolution, Immunity, and Trade-Offs
- Bradford Hill’s Criteria for Causation Applied to LDL Cholesterol and Coronary Heart Disease
- www.vat-trap.com
Related posts
- Cholesterol, LDL, and what we learnt from PCSK9 mutations in familial hypercholesterolaemia
- So what does determine your LDL (‘bad’) Cholesterol?
- LDL: the lower the better
- How to Lose Visceral Adipose Tissue (VAT) and Improve Metabolic Health: A Guide to Sustainable Weight Loss
- Visceral Fat, Mitochondria, and the Energy Trap: Why We Store Fat Where We Shouldn’t
- Why everyone is talking about VAT