An article written by Dr Edward Leatham, Consultant Cardiologist © 2025 E.Leatham
A new SCVC book on personalised metabolic and cardiovascular health
At Surrey Cardiovascular Clinic, one consistent pattern stands out: even when two people share the same diagnosis or the same medication, their bodies respond differently. Appetite, sleep quality, glucose responses, muscle mass, cravings and stress patterns vary widely between individuals.
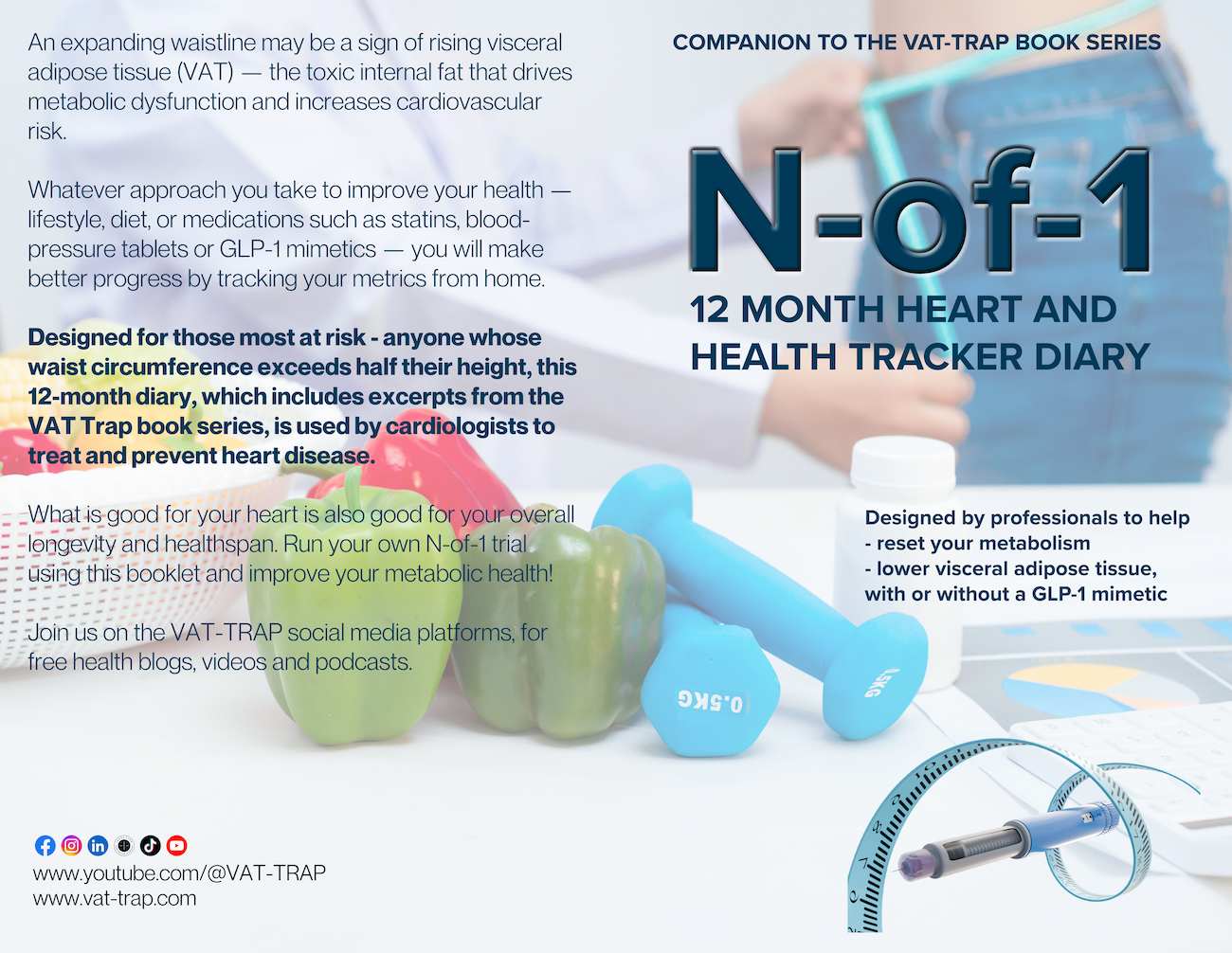
A new 24 page diary — N-of-1 — is written to reflect this reality.
As a companion book in the VAT-TRAP series, N-of-1 introduces the concept of personalised metabolic improvement: you are your own study, your own experiment, your own N-of-1 trial.
What Is an N-of-1 Trial?
Whether you need to lower your blood pressure, weight or waist to improve your metabolic health and healthspan, the N-of-1 technique is a personalised experiment where you:
- change one variable at a time
- observe your own responses
- keep what works
- discard what doesn’t
This mirrors how clinicians personalise treatment daily.
Rather than following generic rules, you work with your own biology — a precision-medicine approach that research increasingly supports¹².
Why This Diary Was Developed
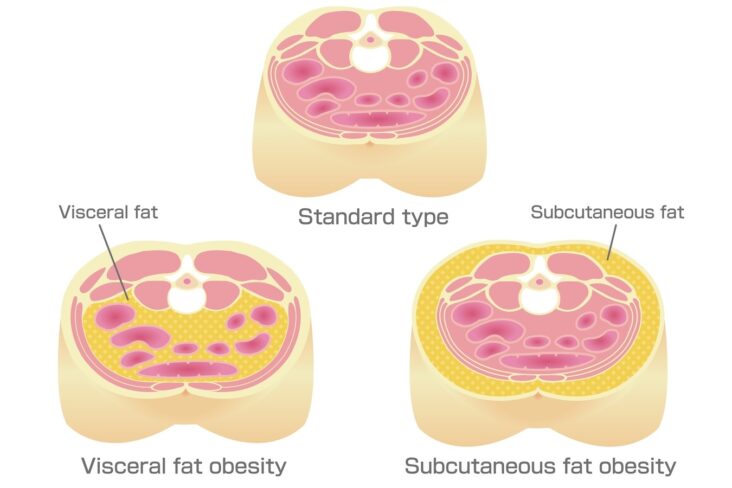
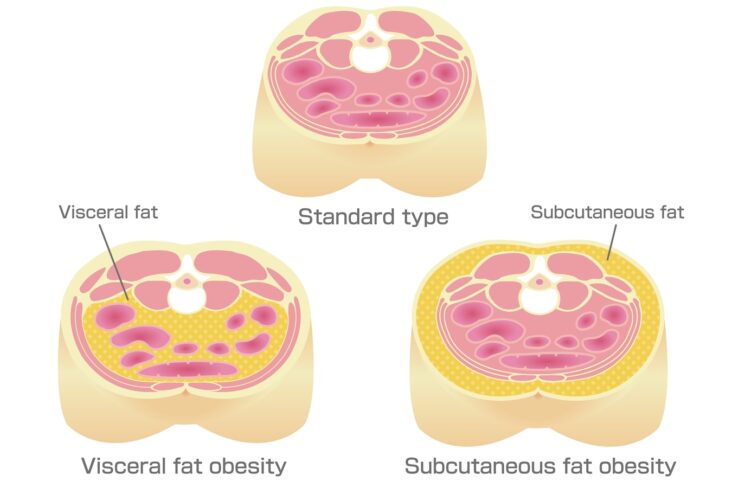
The book series draws on years of cardiology practice treating people with raised visceral adipose tissue (VAT, or belly fat), metabolic drift, glucose variability, weight regain and midlife loss of metabolic flexibility.
A key insight emerged:
Metabolic decline is slow, subtle and often symptomless — and metabolic recovery must be slow, steady and data-guided.
VAT accumulates invisibly over years³⁻⁷.
Sleep disruption, glucose spikes, rising fasting insulin and gradual muscle loss quietly shift the brain’s “defended” weight set point.
Short programmes and rapid weight-loss plans do not reverse these deeper systems.
N-of-1 offers a more realistic path:
a structured, reflective approach that uses small weekly changes to drive measurable long-term improvement.
Why N-of-1 Matters More Than Ever
Modern cardiometabolic science makes this clear:
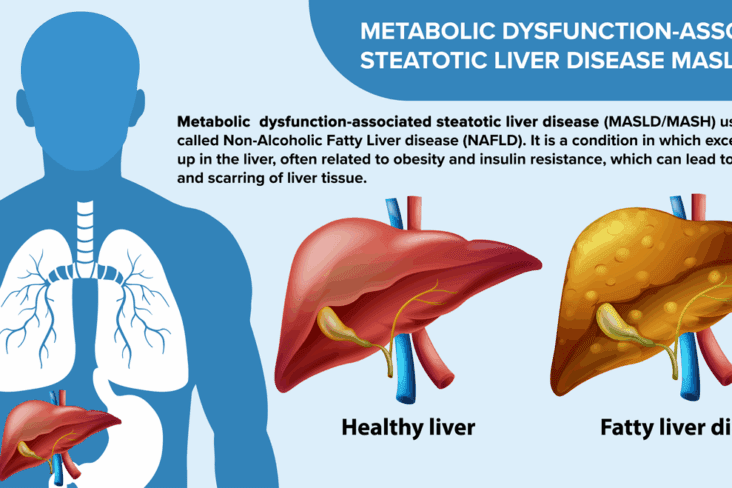
- VAT is a powerful driver of heart disease, metabolic syndrome, dementia and cancer³⁻⁷
- Metabolic dysfunction begins long before diabetes or hypertension appear⁸
- GLP-1 mimetics reduce VAT but require muscle preservation and lifestyle structure⁹
- Tools like CGM, body composition scales and food-analysis apps allow precise early course-correction¹⁰⁻¹¹
N-of-1 shows how to use these tools intelligently — without overwhelm.
What You’ll Learn in the N-of-1 Book
✔ How to run an N-of-1 trial on yourself
Small weekly experiments guided by your own data, not guesswork.
✔ Why slow metabolic change works best
Because VAT biology, mitochondrial function, appetite signalling and liver metabolism adapt gradually⁴⁻⁷.
✔ The four foundations of metabolic reset
- Nutrition
- Movement
- Muscle
- Sleep
Excerpts explain simply and practically.
✔ How to interpret modern metabolic tools
Including glucose responses, body composition, measurement of VAT risk, and understanding GLP-1 effects.
✔ How to build sustainable metabolic habits
Not via intensity or restriction, but by steady repetition, reflection and insight.
Who N-of-1 is For
This book is suitable for:
- anyone with waist-to-height ratio >0.5
- people beginning a 12-month metabolic reset
- patients using GLP-1 mimetics
- individuals noticing midlife metabolic drift
- anyone seeking personalised rather than generic health advice
- those aiming to reduce VAT and improve long-term cardiovascular health
Why Slow Change Is More Effective
Fast approaches often:
- reduce skeletal muscle
- trigger rebound appetite
- lower resting metabolic rate
- accelerate VAT re-accumulation
Slow change allows the body to realign core systems — hypothalamic signalling, insulin sensitivity, muscle glucose uptake and circadian rhythms⁴⁻⁷.
This is the physiological basis for N-of-1:
small, steady improvements beat dramatic short-term efforts.
N-of-1 and GLP-1 Therapy
GLP-1 mimetics such as semaglutide and tirzepatide:
- reduce visceral fat
- improve glucose variation
- lower liver fat
- calm appetite
But they must be paired with nutrition, sleep and resistance training if long-term metabolic stability is the goal⁹.
N-of-1 explains how to integrate medication safely into a sustainable metabolic plan, and how to taper thoughtfully when appropriate.
A Personal Roadmap to Metabolic Health
N-of-1 is not a diet, a challenge or a fixed programme.
It is a mindset — a precision, personalised approach to long-term health.
Using modern tools, weekly reflections and structured self-experimenting, the book helps you understand:
- your metabolic patterns
- your sleep–glucose interactions
- your biological triggers
- your appetite cycles
- your responsiveness to change
You cannot rush metabolic health.
But you can reclaim it — one week, one habit, one experiment at a time.
Learn more at: www.vat-trap.com
Or see the metabolic toolkit page to link to recommended books with a link to the N-of-1 companion diary
References
- Guyatt GH et al. N-of-1 randomized clinical trials in medical practice. BMJ. 2014;348:g3730.
URL: https://www.bmj.com/content/348/bmj.g3730
DOI: 10.1136/bmj.g3730 - Lillie EO et al. The n-of-1 clinical trial: the ultimate strategy for individualising medicine? Per Med. 2011;8(2):161–173.
URL: https://pubmed.ncbi.nlm.nih.gov/21410444/
DOI: 10.2217/pme.11.7 - Neeland IJ et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic risk. JACC. 2019;72(24):2701–2714.
URL: https://www.jacc.org/doi/10.1016/j.jacc.2018.09.042
DOI: 10.1016/j.jacc.2018.09.042 - Fontana L, Eagon JC et al. Effects of weight loss on liver fat, VAT and insulin sensitivity. Diabetes Care. 2005;28:2549–2555.
URL: https://diabetesjournals.org/care/article/28/11/2549/23808
DOI: 10.2337/diacare.28.11.2549 - Britton KA et al. Increased visceral fat and risk of metabolic syndrome. Circulation. 2013;126:1301–1311.
URL: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.111.078998
DOI: 10.1161/CIRCULATIONAHA.111.078998 - Shulman GI. Ectopic fat in insulin resistance, dyslipidaemia and type 2 diabetes. J Clin Invest. 2014;124:415–422.
URL: https://www.jci.org/articles/view/72275
DOI: 10.1172/JCI72275 - Piché ME et al. VAT as an independent cardiometabolic risk factor. Eur Heart J. 2018;39:1185–1193.
URL: https://academic.oup.com/eurheartj/article/39/13/1185/4782404
DOI: 10.1093/eurheartj/ehx648 - Zeevi D et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–1094.
URL: https://www.sciencedirect.com/science/article/pii/S0092867415014217
DOI: 10.1016/j.cell.2015.11.001 - Rubino DM et al. Body composition changes with semaglutide therapy. Lancet Diabetes Endocrinol. 2021;9:809–821.
URL: https://www.thelancet.com/journals/landia/article/PIIS2213-8587(21)00267-8/fulltext
DOI: 10.1016/S2213-8587(21)00267-8 - Thomas MS et al. CGM use in non-diabetic individuals for metabolic insight. Nutrients. 2020;12(9):2624.
URL: https://www.mdpi.com/2072-6643/12/9/2624
DOI: 10.3390/nu12092624 - Thomas DM et al. Home body composition analysis and metabolic tracking. Obesity. 2012;20:108–114.
URL: https://pubmed.ncbi.nlm.nih.gov/22030930/
DOI: 10.1038/oby.2011.331 - Dempsey PC et al. Interrupting sitting with light activity improves glucose control. Diabetes Care. 2016;39:964–972.
URL: https://diabetesjournals.org/care/article/39/6/964/37164
DOI: 10.2337/dc15-2336 - Strasser B, Pesta D. Resistance training and metabolic health. Sports Med. 2013;43:1075–1090.
URL: https://pubmed.ncbi.nlm.nih.gov/23846281/
DOI: 10.1007/s40279-013-0075-x - Spiegel K et al. Sleep curtailment and metabolic dysfunction. Ann Intern Med. 2004;141:846–850.
URL: https://www.acpjournals.org/doi/10.7326/0003-4819-141-11-200412070-00009
DOI: 10.7326/0003-4819-141-11-200412070-00009
Other related articles
- Visceral Fat, Mitochondria, and the Energy Trap: Why We Store Fat Where We Shouldn’t
- How to Lose Visceral Adipose Tissue (VAT) and Improve Metabolic Health: A Guide to Sustainable Weight Loss
- The Expanding Waistline in Men: Spare Tyre, Killer Visceral Fat, or Just Flabby Abdominal muscles?
- GLP-1 mimetic clinic
- Effects of different exercise types on visceral fat in young individuals with obesity aged 6–24 years old: A systematic review and meta-analysis 2022
- Clinical significance of visceral adiposity assessed by computed tomography: A Japanese perspective: 2014
- From Genes to Greens: How DNA Shapes Your Nutritional Needs
- Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement 2019
- Body fat distribution on computed tomography imaging and prostate cancer risk and mortality in the AGES-Reykjavik study 2019