An article written by Dr Edward Leatham, Consultant Cardiologist
Tags: DNA, Nutrition, NH1 search website using Tags to find related stories.
Nutrigenomics is the science that studies how our genes interact with nutrients. DNA testing can now identify specific gene polymorphisms – small variations in DNA – that affect how we absorb, metabolise, and utilise key macro- and micronutrients.
For example:
- FTO and MC4R genes are associated with how your body stores fat and responds to satiety cues.
- MTHFR polymorphisms can impact folate metabolism and methylation, influencing energy, mood, and cardiovascular risk.
- Variants in CYP1A2 determine how quickly you metabolise caffeine, which has implications for blood pressure and sleep.
- LCT gene status indicates lactose tolerance – critical when considering dairy as a calcium source.
Armed with this information from a Nutrinomix DNA test your doctor or nutrition specialist can fine-tune your diet to your genetic strengths and vulnerabilities – whether that means increasing certain B vitamins, moderating your fat intake, or choosing slower-digesting carbohydrates.
CGM Monitoring and Food Analysis Apps: Real-Time Nutrition Insights
Your DNA tells you what might happen – but continuous glucose monitors (CGMs) and digital food tracking apps show you what is happening in real time.
Even in people without diabetes, CGMs reveal fascinating inter-individual differences in how foods affect blood glucose. For example, one person may have a significant glucose spike after eating oats, while another doesn’t. These variations can’t always be predicted by the glycaemic index alone – they’re the product of your gut microbiome, insulin sensitivity, and even your stress levels.
By combining CGM data with AI-powered food tracking apps, you can build a picture of:
- Which meals keep your glucose stable
- Which foods lead to energy crashes or cravings
- How your body responds to fasting, exercise, or poor sleep
This phenotypic feedback loop allows you and your doctor to refine your food choices not only based on theory, but on actual metabolic response.
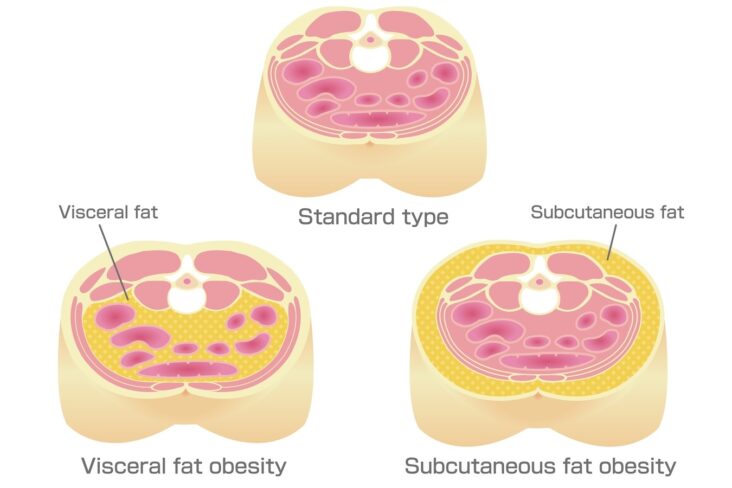
Seeing Beneath the Surface: DEXA and Low-Dose CT Scans
You might weigh 70 kg – but what’s inside that number matters far more than the number itself. Advanced body composition scans offer precise insights into your inner health.
DEXA (Dual-Energy X-ray Absorptiometry):
This scan provides detailed data on:
- Visceral fat – the dangerous fat stored around abdominal organs, often hidden despite a “normal” BMI
- Lean muscle mass – critical for metabolic function and long-term strength
- Bone mineral density – key for assessing fracture risk and osteoporosis
Low-Dose CT Scans:
While DEXA is excellent for body composition trends, low-dose CT scanning offers even more precision in quantifying visceral fat volume – the fat that wraps around your liver, pancreas, and intestines. This type of fat is strongly associated with insulin resistance, inflammation, and cardiovascular disease risk. For examples see related blog.
It’s this “hidden fat” – not the fat under your skin – that contributes most to the middle-age spread and derails metabolic health. As we age, we also tend to lose skeletal muscle, which plays a key role in glucose disposal and maintaining insulin sensitivity. Together, increased visceral fat and declining muscle mass form the perfect storm for metabolic dysfunction, leading to:
- Central obesity
- Pre-diabetes and type 2 diabetes
- Fatty liver disease
- Accelerated cardiovascular ageing
With a low-dose CT scan, doctors can visualise and quantify this fat burden with remarkable accuracy – and target it in your health plan.
Epigenetics: Lifestyle Imprints on Your Genes
One of the most powerful concepts in modern medicine is that genes are not destiny. Through processes called epigenetics, your environment, diet, stress levels, and activity can switch genes on or off.
What you eat, how well you sleep, your exposure to toxins, even your thought patterns – all leave molecular marks on your DNA that influence gene expression. These changes can alter your risk of disease, inflammation levels, metabolic function, and even ageing speed.
By combining DNA polymorphism analysis (your inherited blueprint) with CGM, food tracking, DEXA, CT scans, and other phenotype data (your expressed characteristics), we can map out your epigenetic terrain – the current state of your health as shaped by both genes and lifestyle.
The Future: A Personalised Health Profile for Each Patient
The promise of this integrated approach is a personalised health profile – a living, breathing document that evolves with you.
With your doctor’s guidance, it might include:
- Gene-based dietary recommendations
- A food and glucose response map based on CGM trends
- A visceral fat and muscle mass trajectory
- Sleep and stress metrics
- A roadmap to reduce your biological age and disease risk
This isn’t just about prevention – it’s about optimisation. Whether your goal is more energy, sharper cognition, weight loss, better metabolic health, or longevity, these tools offer a tailored strategy based on your biology, not population averages.
The Cardiologist’s View: Precision Profiling in Patients Over 40
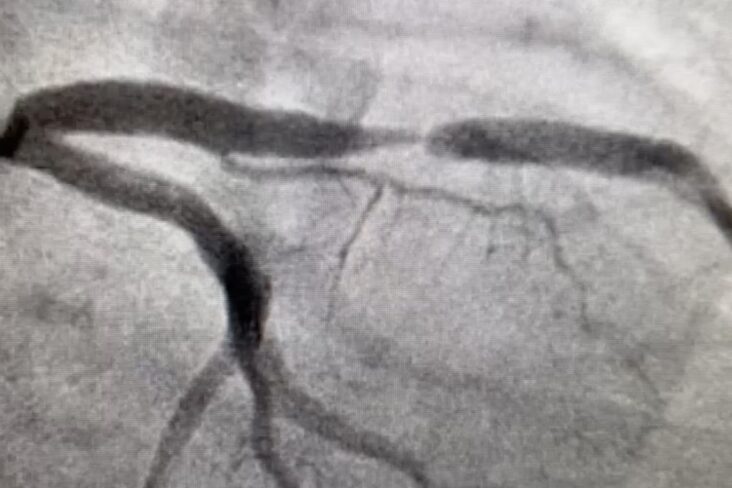
From a cardiologist’s perspective, these advanced investigations are particularly relevant in patients aged 40 and above, when subtle but significant cardiovascular changes often begin to emerge. Many of our patients will have already undergone a coronary CT scan with FAI (Fat Attenuation Index) — an advanced imaging technique that not only visualises coronary plaque but also quantifies:
- Location and burden of atherosclerotic plaque
- Degree of calcification
- Localised inflammation in each coronary vessel
FAI analysis provides powerful prognostic information, helping to identify patients at high risk of fatal myocardial infarction (MI) within the next 8 years — even when traditional risk scores appear low or intermediate.
This data-driven approach enables stratification of cardiovascular risk with far greater precision. By integrating genomic, metabolic, and phenotypic data — including DEXA, low-dose CT for visceral fat, CGM for glycaemic patterns, and food response analytics — we can prioritise both pharmacological and lifestyle interventions. For high-risk patients, this might include early use of lipid-lowering agents, targeted nutritional adjustments, visceral fat reduction strategies, and muscle-preserving exercise prescriptions.
Ultimately, the aim is not just to reduce cardiovascular events, but to improve healthspan — the years lived free from disease and functional decline — through a personalised, proactive approach to prevention.
The Takeaway: Own Your Data, Own Your Health
We are at the frontier of a new era in medicine – one where your own data becomes the foundation of your care. When used responsibly and under professional guidance, DNA testing, food analysis apps, CGM, DEXA, and low-dose CT scans empower you to make smarter, more targeted decisions about your health.
Instead of trial-and-error or generic advice, you can now ask: What does my body need? And get an answer that’s backed by evidence and personalised to you.
Your healthspan – and your quality of life – depend on it.
Other related articles
- The Expanding Waistline in Men: Spare Tyre, Killer Visceral Fat, or Just Flabby muscles?
- Dietary Fats: From Villain to Vital Nutrient – Rethinking Fat in a Heart-Healthy Diet
- The 8-Month Metabolic Reset: A New Approach to Reversing Visceral Fat, Improving Blood Pressure and Blood Glucose
The Naked Heart is an educational project owned and operated by Dr Edward Leatham. It comprises a series of blog articles, videos and reels distributed on Tiktok, Youtube and Instagram aimed to help educate both patients and healthcare professionals about cardiology related issues.
If you would like to receive email notification each week from the Naked Heart, follow me on social media or please feel free to subscribe to the Naked Heart email notifications here