An article written by Dr Edward Leatham, Consultant Cardiologist
Tags: VAT, CGM, Metabolic health, Diabetes, NH1, search website using Tags to find related stories.
For busy people, or to tune in when on the move, Google Notebook AI audio podcast and an explainer slide show are available for this story beneath.
“For every threat that rises against us, humanity answers with a greater invention. Show us the enemy, and we will forge the remedy.”
For much of modern cardiology, in its battle against coronary artery disease—one of mankind’s greatest threats—the “enemy” seemed clear. When I trained, the diagnostic armoury was focused on accurately identifying flow-limiting narrowing of one or more coronary arteries: the 3–4 mm caliber vessels supplying the heart with oxygenated blood. Prognosis was measured by the number of occluded arteries, the degree of stenosis, left ventricular ejection fraction, blood pressure, and cholesterol profile. Secondary prevention was simply a junior aspirin, a statin and adequate blood pressure control.
Diabetes mellitus was acknowledged as a risk factor, but it was largely regarded as a separate, niche condition—managed primarily by GPs and endocrinologists. Invasive coronary angiography was the gold standard, the reference point against which all non-invasive tests—such as the stress ECG or nuclear cardiology scans—were judged. A patient’s future could be read from the arteries illuminated on that cath lab screen: a narrowing meant risk; an occlusion demanded action.
Yet in the last decade, a profound paradigm shift has unsettled these foundations—and in some respects, turned them on their head.
The Shift from Narrowings to Inflammation and Metabolism
Yes, left ventricular function and LDL cholesterol remain critical. But the discovery that, outside the specific clinical scenario of an acute coronary syndrome, where a prompt invasive angiogram with option for the fitting of a stent is mandatory , future coronary thrombosis is driven less by the degree of narrowing and far more by the degree of inflammation within a plaque has been revolutionary 7–11. Similarly, cardiovascular prognosis is no longer tied only to whether a patient crosses the arbitrary diagnostic threshold for diabetes. Instead, it is linked to a continuum of glucose dysregulation, measurable across the full HbA1c spectrum. Put simply: the lower your HbA1c, the better your cardiovascular outlook—even in the absence of a formal diabetes diagnosis.
This discovery reframes metabolic health as the central battlefield of cardiovascular prevention.
The Power of Glucose-Lowering Drugs Beyond Diabetes
In the last decade, large-scale trials have confirmed that certain glucose-lowering therapies confer survival benefits even in non-diabetic patients.
- SGLT2 inhibitors have shown unequivocal improvement in outcomes for patients with heart failure, irrespective of diabetic status 1–3.
- In 2023, the landmark semaglutide trial demonstrated that GLP-1 receptor agonists offer striking survival benefits for non-diabetic patients with coronary heart disease 4–6.
These findings mean that the threat we now face is not “diabetes” per se, but metabolic dysfunction—spanning obesity, visceral adiposity, insulin resistance, and disordered glucose handling. Type 2 diabetes and obesity are not just metabolic inconveniences; they are the rising tide threatening global cardiovascular and healthcare systems alike.
A Renaissance in Cardiovascular Medicine
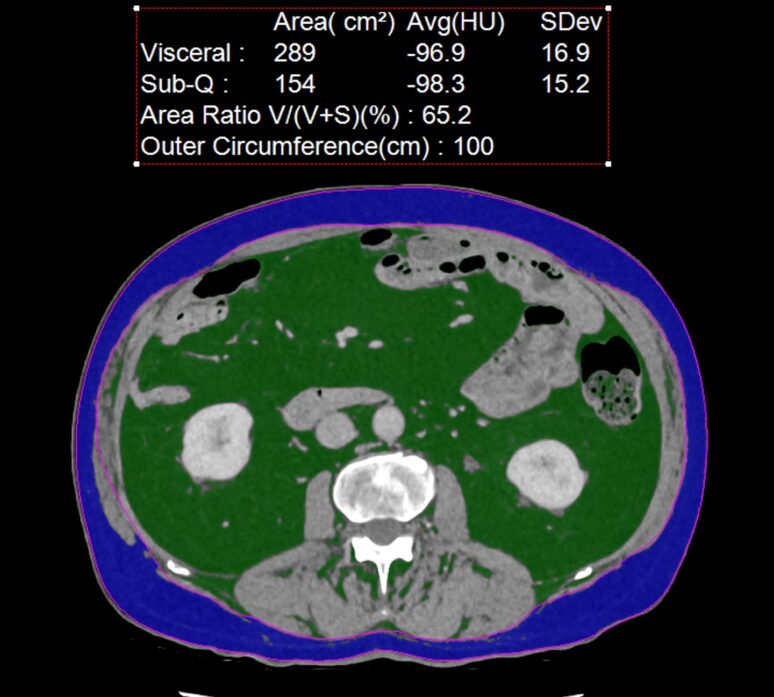
Armed with this new knowledge—and crucially, with new therapeutic firepower—cardiologists are re-orienting their practice. We have a newly identifiable enemy: poor metabolic health, and new tools to identify threats earlier than ever before. AI-guided data processing from cardiac CT images can now provide insight into the degree of coronary inflammation (and thus risk) as long as a decade before any symptoms develop. Continuous glucose monitoring (CGM) technology allows us to identify non-diabetic hyperglycaemia well before the HbA1c drifts into a “pre-diabetic” range. Low-dose CT can be used to detect high levels of visceral adipose tissue (VAT)—even in patients with a normal BMI—that drives insulin resistance and poor metabolic health.
Once a threat is identified, next generation, multidisciplinary cardiometabolic clinics have an array of non-pharmacological strategies to counter a better-defined enemy. CGMs, combined with patient education, can tailor food intake to avoid glucose highs in the carbohydrate-sensitive. Food analysis apps can guide patients towards healthier macronutrient proportions. DNA testing can identify polymorphisms linked to macro- and micronutrient vulnerabilities.
Tracking progress in any “health war” is paramount. Patients need to see incremental progress in a positive direction, which reinforces behavioural changes such as improved eating patterns, resistance training, and high-intensity interval training (HIIT). This starts with a simple waist measurement but, depending on risk and patient engagement, can be extended to include home body-composition scales, DEXA body-composition scans, and periodic low-dose CT to measure VAT.
Where progress with conventional lifestyle measures, diet, and simple therapies such as statins stalls or fails, potent pharmacological treatments are now available in the cardiologist’s arsenal. These include PCSK9 inhibitors, SGLT2 inhibitors, and GLP-1 mimetics.
This shift is not only scientific but also psychological, and this psychological impact is often the catalyst for behavioural change.
Population studies have long shown us that expanding waistlines and raised cholesterol levels increase risk. Yet many patients continued to believe that heart disease was something that afflicted “older, other people.” Nothing shatters this illusion more than sitting with your cardiologist, viewing your coronary CT on a large screen, and seeing a vividly inflamed plaque in the proximal left anterior descending artery—the so-called “widow-maker.” At that moment, when attention is inevitably drawn to the CaRi heart score dashboard showing a 15% eight-year mortality risk without intervention, the reality becomes undeniable.
The ability to visualise coronary plaque, quantify its characteristics, and assess inflammation of surrounding fat using the Fat Attenuation Index (FAI) represents one of the great advances in preventive cardiology. Coupled with CGMs revealing that many “non-diabetic” patients experience alarming glucose spikes after high-glycaemic foods, cardiologists now have powerful new diagnostic tools to complement the traditional ECG, echocardiogram, lipid profile, and invasive angiography.
The message is clear: the battlefield has moved upstream—into the realm of inflammation and metabolism.
Why “Primary” and “Secondary” Prevention No Longer Fit
Twenty years ago, the terminology of prevention was simple:
- Primary prevention was the GP’s domain, keeping healthy people healthy through lifestyle advice, blood pressure control, and statins.
- Secondary prevention was the cardiologist’s remit, treating patients who had already suffered an infarct or undergone stenting or bypass.
Today, the picture is less neat. A patient with no symptoms but extensive coronary plaque on CT, a high FAI, or clear metabolic dysfunction is at as great a risk of cardiovascular death as someone who has already had a first heart attack. Starting statins or GLP-1 therapy in such a patient is not really “primary prevention” at all.
The traditional binary has collapsed. The terms feel outdated and increasingly misleading. Prevention is now a continuum, and cardiologists are leading this redefinition.
Family History, Cancer, and the Expanding Scope of Prevention
For decades, family history guided much of our preventive focus. A family tree heavy with myocardial infarction, need for coronary artery bypass surgery or stent justified aggressive lipid lowering. In contrast, if cancer dominated the family history, the rationale for aggressive statin therapy felt weaker.
But this too is shifting.
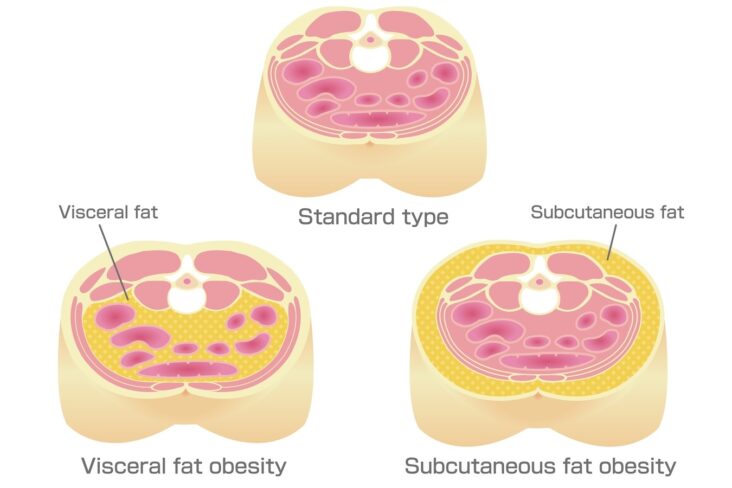
Visceral adiposity—now measurable via low-dose CT—is emerging as a potent risk factor for both cardiovascular disease and cancer12–14. An asymptomatic patient found to have:
- Extensive coronary plaque,
- Non-diabetic hyperglycaemia on CGM, and
- A visceral adipose tissue (VAT) burden exceeding 200 cm²
is not just facing a cardiovascular time bomb but also an greatly elevated cancer risk.

A CT scan of the abdomen at L3 can be used identify visceral fat (in green) that is metabolically active causing insulin resistance and which is an independent and major risk factor for both cardiovascular diseases and certain cancers. In this example the VAT score of 289 cm2 is well over the healthy threshold of 100 cm2 .
Interventions such as dietary restructuring, resistance training, and GLP-1 mimetic therapy now promise to reduce both cardiovascular and oncological risks simultaneously. In this sense, cardiologists are thus moving into the realm of longevity medicine.
Two Routes into the New Paradigm
Patients are entering this new landscape through two main routes:
- Symptom-driven investigations
Patients presenting with chest pain, breathlessness, palpitations, or other concerning symptoms are increasingly investigated not only with echocardiograms and ECGs, but also with coronary CT scans, FAI assessment, VAT measurement, and metabolic profiling. - Proactive health screening
A growing number of health-conscious individuals are accessing advanced screening packages. For employers, offering annual checks that include cardiac CT, CGM analysis, and VAT measurement can be highly tax-efficient while enhancing workforce health. For individuals, the appeal is obvious: detect risk before it manifests, and intervene before it is too late.
From Stents to Prevention: A Personal Perspective
For interventional cardiologists trained in the cath lab, this shift has been nothing short of transformative. Where once our lives revolved around wires, balloons, and stents, now our clinics revolve around metabolic profiling, lifestyle intervention, and preventive pharmacology.
I often tell patients: “I used to stent. Now I prevent.”
It is not a retreat from cardiology’s core mission, but an expansion. Where once we fought the visible narrowing, we now fight the invisible metabolic dysfunction that fuels both cardiovascular disease and cancer.
Conclusion: The New Enemy, the New Arsenal
The identifiable enemy of 21st-century cardiology is not simply obstructive coronary stenosis. It is the insidious triad of poor metabolic health, visceral adiposity, and chronic inflammation.
Our weapons are no longer confined to stents and statins. We now wield:
- Coronary CT with plaque characterisation and FAI,
- Continuous glucose monitoring,
- VAT assessment,
- GLP-1 mimetics and SGLT2 inhibitors,
- Intensive lifestyle and nutritional interventions.
The traditional language of primary and secondary prevention no longer captures this reality. Prevention is no longer two separate categories—it is a spectrum of risk requiring earlier, more personalised, and more aggressive action.
We stand at the threshold of a cardiovascular renaissance. The future of cardiology will not be written solely in catheter labs but also in consultation rooms, nutritional plans, and metabolic clinics.
The principle enemy may not have changed but it has new facets we can measure more accurately and our diagnostic and treatment arsenal has changed. In forging ahead with these new remedies, cardiologists may well become the clinicians of longevity itself.
References
- Kommu S. The role of SGLT2 inhibitors on heart failure outcomes in patients without diabetes mellitus. 2024.
- Teo YH, et al. Effects of SGLT2 inhibitors in patients without diabetes mellitus with heart failure: a 20% relative risk reduction in heart failure outcomes. J Am Heart Assoc. 2021.
- McMurray JJV, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction (DAPA-HF trial): both diabetic and non-diabetic cohorts saw reduced CV death and HF hospitalization. Circulation. 2019.
- Lincoff AM, et al. Semaglutide and cardiovascular outcomes in obesity; effects beyond glycaemic control. N Engl J Med. 2023.
- Deanfield J, et al. SELECT trial: Once-weekly subcutaneous semaglutide in overweight or obese patients with established cardiovascular disease but without diabetes: 20% reduction in MACE over ~33 months. 2024.
- Abdeen M, et al. Cardiovascular effects of GLP-1 receptor agonists, especially semaglutide, in non-diabetic adults with obesity: systematic review. Presented May 2025.
- Oikonomou EK, Desai MY, Marwan M, et al. Perivascular fat attenuation index stratifies cardiac risk associated with high-risk plaques in the CRISP-CT study. J Am Coll Cardiol. 2020;76(6):755–757.
- Antoniades C, Kotanidis CP, Berman DS. Atherosclerosis affecting fat: What can we learn by imaging perivascular adipose tissue? J Cardiovasc Comput Tomogr. 2019;13(5):288–296.
- Goeller M, Achenbach S, Cadet S, et al. Pericoronary adipose tissue computed tomography attenuation and high-risk plaque characteristics in acute coronary syndrome compared with stable coronary artery disease. JAMA Cardiol. 2018;3(9):858–863.
- Oikonomou EK, Marwan M, Desai MY, et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP-CT study): a post-hoc analysis of prospective outcome data. Lancet. 2018;392(10151):929–939.
- Pericoronary fat attenuation index—a new imaging biomarker and predictor of cardiovascular events. Eur Heart J Cardiovasc Imaging. 2022;23(12).
- Ruiz-Castell M, et al. Estimated visceral adiposity is associated with chronic metabolic and cardiovascular disorders: a CT-based study. Sci Rep. 2021;11:12345.
- Britton KA, et al. Body fat distribution and incident cardiovascular disease: focus on visceral adiposity. J Am Coll Cardiol. 2013;61(5):490–499.
- Silveira EA, et al. Visceral obesity by CT scan and incident cardiovascular disease and cancer risk: a longitudinal cohort analysis. Cancers. 2020;12(4):988.
- Shah VN, et al. Continuous glucose monitoring profiles in healthy individuals. J Clin Endocrinol Metab. 2019;104(10):4356–4364.
- UCL Review. Continuous glucose monitoring may offer significant potential benefits for cardiovascular prevention in healthy individuals. Eur J Prev Cardiol. 2025;32(Suppl 1):zwaf236.280.
- University College London, Birmingham Children’s Hospital. Evaluating CGM accuracy and benefits in people not living with diabetes. Diabet Med. 2024.
- Breakthrough T1D. CGMs may detect subclinical dysglycemia in overweight or high-risk non-diabetic individuals. Breakthrough T1D News. 2025.
- The Guardian. I’m not diabetic—should I be using a glucose monitor? 11 March 2024.
- Hanssen MJN, Kraakman MJK, Flynn MC, et al. Postprandial glucose spikes: an important contributor to cardiovascular disease in diabetes? Front Endocrinol (Lausanne). 2020;11:254.
- Belli M. Glucose variability: a new risk factor for cardiovascular disease? Diabetes Metab Syndr Clin Res Rev. 2023.
- Hjort A, et al. Glycaemic variability assessed using continuous glucose monitoring is a strong risk factor for cardiovascular events in patients with stable angina. Atherosclerosis. 2024.
- Attia P. Individuals in highest 20% of postprandial glucose responses had 2.7× higher risk of cardiovascular mortality over 20 years. PeterAttiaMD.com. 2023.
Other related articles
- Why the Mediterranean Diet Works: It’s More Than Just What You Eat
- Why everyone is talking about VAT
- How to Lose Visceral Adipose Tissue (VAT) and Improve Metabolic Health: A Guide to Sustainable Weight Loss
- The 8-Month Metabolic Reset: A New Approach to Reversing Visceral Fat, Improving Blood Pressure and Blood Glucose
- Five Reasons Why a Cardiologist Might Recommend a Continuous Glucose Monitor (CGM) to their Patient
The Naked Heart is an educational project owned and operated by Dr Edward Leatham. It comprises a series of blog articles, videos and reels distributed on Tiktok, Youtube and Instagram aimed to help educate both patients and healthcare professionals about cardiology related issues.
If you would like to receive email notification each week from the Naked Heart, follow me on social media or please feel free to subscribe to the Naked Heart email notifications here