An article written by Dr Edward Leatham, Consultant Cardiologist
For busy people on the move, Google Notebook AI audio podcast and an explainer slide show are available for this story beneath.
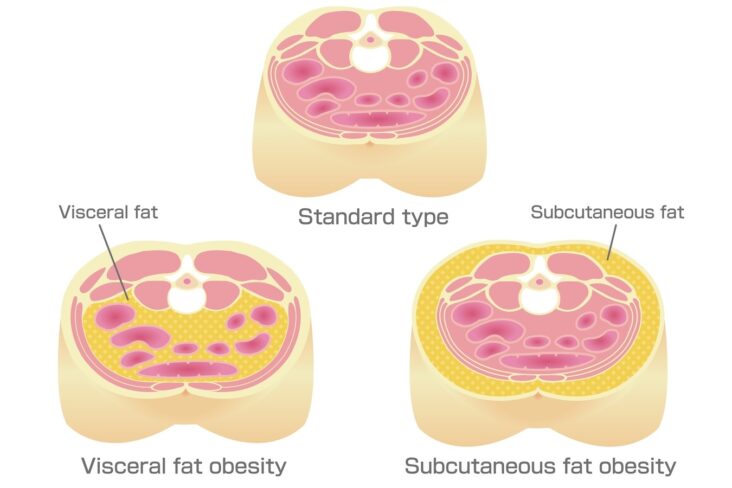
Visceral adipose tissue (VAT) is the fat that surrounds the internal organs, particularly within the abdominal cavity. Unlike the fat just under the skin, VAT is not merely a cosmetic concern—it has a profound impact on metabolic health. Excess VAT is strongly linked to conditions such as insulin resistance, type 2 diabetes, cardiovascular disease, and even certain cancers. For this reason, reducing visceral fat is a key goal for anyone aiming to improve metabolic health and/or to achieve sustainable weight loss.
For patients with conditions associated with raised VAT, effective pharmacological options are now available. GLP-1 receptor agonists—such as semaglutide or tirzepatide—promote weight loss, reduce VAT, and improve blood sugar control without increasing the risk of hypoglycaemia. A secondary benefit is a reduction in HbA1c levels.
While these medications can be transformative, combining them with targeted lifestyle strategies appears to be essential to maximum their benefit and minimize the risk of complications such as sarcopenia (muscle loss leading to fraily). A proactive approach not only enhances the results but can also reduce the need for long-term medication. In this blog post, we will explore the evidence-based strategies used in our cardiometabolic clinic to reduce VAT, improve metabolism, and also support long-term weight management when needed—whether you are:
taking GLP-1 therapy and wish to maximise its benefits
aiming to reduce your dependence on medication
or seeking to lose visceral fat without pharmacological assistance.
The Growing Focus on Targeting Glucose and Metabolic Health in Cardiology
In recent years, large clinical trials have shown that GLP-1 receptor agonists and SGLT2 inhibitors not only improve glucose control but also enhance metabolic health and reduce cardiovascular risk. These findings are reshaping cardiology practice, with growing recognition that targeting glucose metabolism and visceral fat loss can significantly benefit patients across a wide spectrum of heart conditions. These include hypertension, atrial fibrillation, heart failure, sleep apnoea, and coronary heart disease—both in patients with and without diabetes—as well as those looking to improve longevity and healthspan.
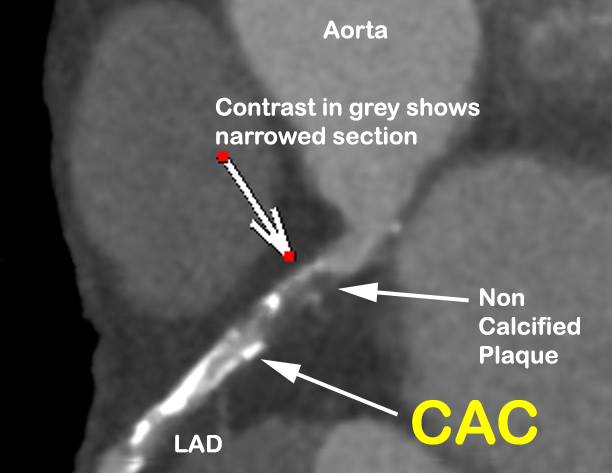
Traditionally, cardiology has focused on managing heart disease through medication, procedures, and hospital-based care. Now, with robust evidence and the availability of digital tools that help optimise glucose levels and track visceral fat loss, there is a clear shift towards integrated care. This approach combines lifestyle and dietary interventions with pharmacological strategies such as GLP-1 therapy, creating a more holistic plan for managing cardiovascular and metabolic health. For patients with coronary artery disease, sleep apnoea, heart failure, or atrial fibrillation, improving glycaemic control and reducing visceral fat can have a transformative impact—not just on symptoms, but also on long-term prognosis.
Reflecting this change, many cardiology groups, including ours, are now partnering with diabetes and weight-management specialists to establish GLP-1 clinics. These services actively monitor visceral fat reduction, support glucose optimisation, and tailor treatment to each patient’s needs. The aim is not only to control symptoms but also to target the root drivers of cardiovascular risk, reduce reliance on multiple medications, and improve overall quality of life.
The Importance of Keeping a Diary to Track Progress
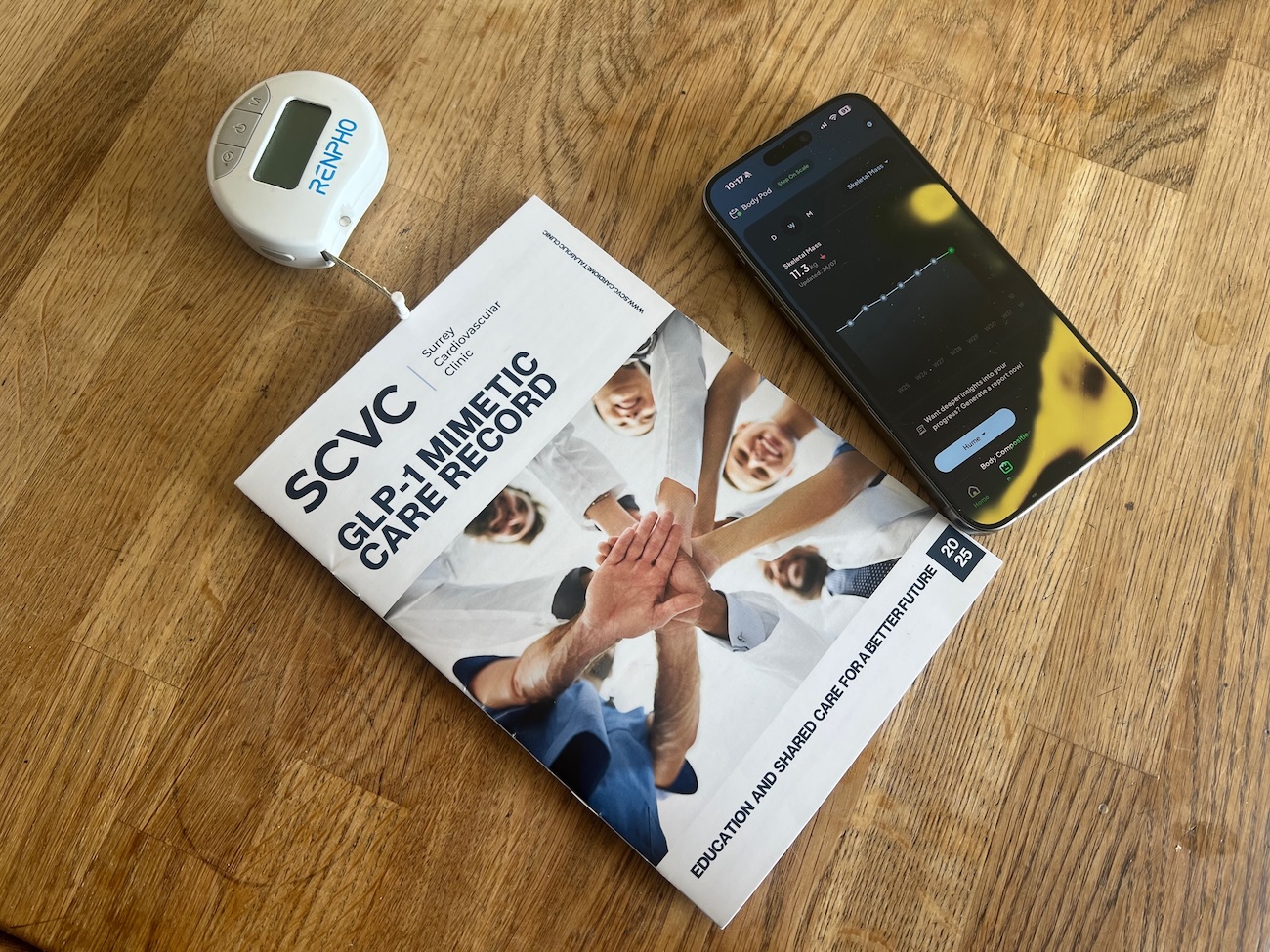
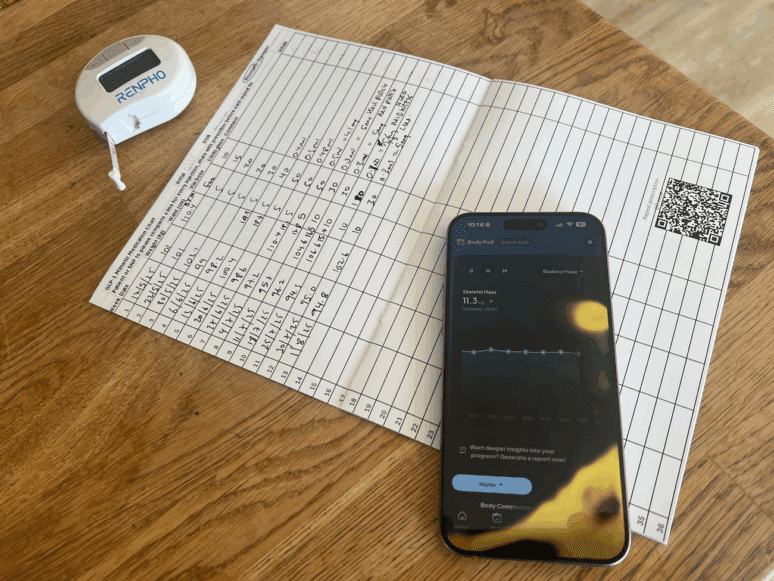
Whether you are aiming to lose weight, reduce visceral adipose tissue, or improve your metabolic health through lifestyle and dietary interventions—with or without GLP-1 mimetic injections—it is very useful to track progress in a diary. Keeping a record of your weight, waist circumference (and GLP-1 medication dose) can help you stay focused, identify patterns, and make adjustments to your plan as needed. While there are plenty of modern apps out there to assist in this effort, including wearable technology such as the Oura ring, Apple and Withings watches, there is nothing quite as good as a paper based diary that you can share with your health team and health record using your smartphone!
In our GLP-1 mimetic clinic, we issue all patients with a shared care booklet, which we ask them to bring to each appointment. We incentivise ‘homework’ by requiring photographs of the central page (see below) to chart progress and which is a prerequisite for repeat prescribing within an 8 month package. It has long been established that a shared care record reduces the number of medical appointments and duplication of effort (ie time and cost). By making the shared care booklet a basic minimum requirement within the programme, we reinforce the need for a routine and some extra discipline needed to achieve sustained success. By tracking progress for themself, our patients also get ownership and become more involved in the decisions about their health journey, which we believe may help reduce the need for long-term GLP-1 mimetic medication.

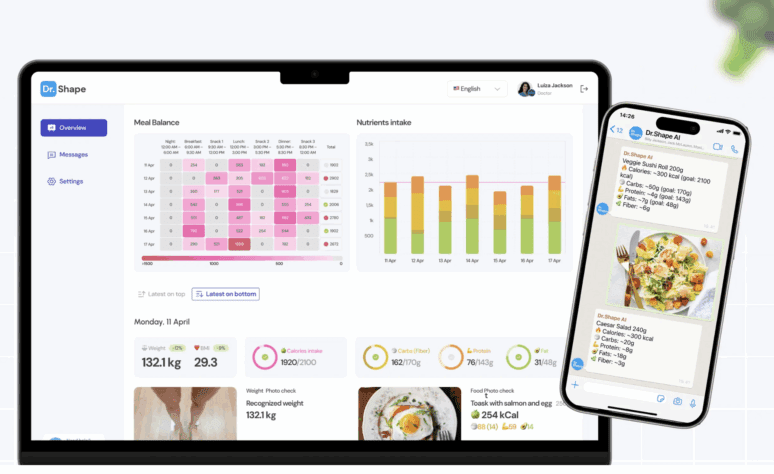
All patients attending our GLP-1 mimetic clinic are given a shared care record and encouraged to use home monitoring technology to track their progress. Instead of maintaining a traditional food diary, we streamline the process by offering a smartphone-based food and weight tracker. This tool uses AI to automatically analyse meals and calculate daily macronutrient intake—protein, carbohydrates, fat—as well as total calories. Matching these macronutrient targets is particularly important when making dietary changes aimed at reducing visceral adipose tissue (VAT), as each plays a role in influencing fat distribution and metabolic health.

More information about this technology see our Metabolic Toolkit page.
Caloric Restriction: The Power of Smaller Plates
Caloric restriction is a fundamental principle in any weight loss plan, and it plays a key role in reducing VAT. One simple technique is to use smaller plates. This can help control portion sizes and prevent overeating. Smaller plates tend to encourage people to eat less, even though they may not feel deprived. This trick helps with portion control and can lead to an automatic reduction in caloric intake without requiring drastic changes to the types of foods you consume.
In addition to smaller portions, it’s important to focus on nutrient-dense foods that are lower in calories but high in fibre, vitamins, and minerals. Vegetables, lean proteins, and healthy fats should be incorporated into each meal. Remember, weight loss doesn’t require deprivation—it’s about making smarter choices that contribute to a healthier body.
Balanced Plate: The Harvard Plate Model
To ensure you’re getting the right balance of nutrients, consider using the Harvard Plate model. This method recommends that your plate should be divided into three sections: half for vegetables, a quarter for lean protein, and a quarter for whole grains or complex carbohydrates. This balance of food groups helps regulate your blood sugar levels, reduce cravings, and provide your body with the essential nutrients it needs to function optimally.
Vegetables are rich in fibre, which helps to promote satiety and improve digestion, while lean proteins such as chicken, fish, or plant-based options like beans and lentils help to build and repair muscle tissue. Whole grains like quinoa, brown rice, and oats provide slow-digesting carbohydrates that stabilise blood sugar, which is especially beneficial for those using GLP-1 mimetics to manage glucose levels.
Increase Intake of Satiety-Inducing Fats
Including healthy fats in your diet can help you feel full and satisfied, which reduces the temptation to overeat. Focus on unsaturated fats, which have been shown to promote heart health and support weight loss. Foods such as avocados, olive oil, oily fish (like salmon and mackerel), and nuts are excellent sources of unsaturated fats.
These fats not only provide essential nutrients but also help regulate hormones that control hunger. Incorporating these healthy fats into your meals can improve your overall dietary satisfaction, making it easier to stick to a reduced-calorie diet without feeling deprived.
Ensure Sufficient Protein Intake
Protein is an essential macronutrient for muscle building and repair, and it plays a key role in weight loss. The Recommended Daily Intake (RDI) for protein is 0.8 grams per kilogram of body weight, but this may need to be increased to 1.2 grams per kilogram or more if you are on a weight loss programme or engaging in resistance training.
Ensure that every meal contains a good source of protein, whether from animal or plant-based sources. Lean meats, fish, eggs, tofu, legumes, and dairy products are all great options. Using a food tracking app such as Dr. Shape can help you monitor your protein intake and ensure you’re meeting your goals.
The Myth of Avoiding Dairy and Fats to Lower Cholesterol
There has long been a common belief that avoiding dairy products and fats is necessary to lower cholesterol levels and reduce the risk of heart disease. However, this myth has now been largely debunked. In fact, heart disease is less prevalent in populations that consume dairy products, and studies have shown that the consumption of full-fat dairy does not appear to have a significant impact on cholesterol levels or heart disease risk.
LDL cholesterol, often referred to as “bad” cholesterol, is the principal cause of coronary artery disease (CAD), but it is important to note that only about 10% of LDL cholesterol levels are influenced by diet. The remaining 90% of LDL cholesterol levels are genetically determined, meaning that your genes play a much larger role in determining your cholesterol levels than your diet does.
As a result, many experts now recommend including eggs, dairy, and healthy fats, such as those found in olive oil, avocado, and nuts, in your diet. These foods provide essential nutrients and help support overall health. The main dietary culprits when it comes to heart disease are refined carbohydrates and sugars, not fats. High sugar intake, particularly from processed foods, is far more likely to contribute to heart disease and metabolic issues than the consumption of whole foods like dairy and eggs.
Increase Water Intake
Water is often overlooked in weight loss plans, but adequate hydration is crucial for both fat loss and the effectiveness of GLP-1 mimetics. Drinking water before meals can help to increase satiety, reducing the likelihood of overeating. Water also supports the metabolism and enhances the ability of GLP-1 mimetics to regulate glucose levels and promote fat loss.
Aim to drink at least 2-3 litres of water per day, and more if you are engaging in physical activity or are in a hot climate. Herbal teas and water-rich foods such as fruits and vegetables can also contribute to your daily fluid intake.
Moderate Alcohol Intake
While the occasional glass of wine or beer isn’t inherently bad, excessive alcohol consumption can significantly hinder fat loss efforts. Alcohol is calorie-dense and often consumed in excess, contributing to increased caloric intake and fat storage, particularly in the abdominal area.
Excess alcohol can also lead to poor food choices and decreased motivation to exercise, which can further derail weight loss efforts. If you want to lose visceral fat and improve metabolic health, it’s essential to moderate alcohol intake and be mindful of its impact on your overall health goals.
Adequate Movement: Aim for 10,000 Steps a Day
Physical activity is a cornerstone of fat loss, and it is essential to target visceral fat. While aerobic exercises such as walking, running, and cycling are beneficial, it’s important to incorporate more movement into your daily life. Aiming for 10,000 steps a day is an effective goal that can help burn calories and improve cardiovascular health.
In addition to walking, consider increasing the intensity of your workouts to maximise fat loss. High-intensity interval training (HIIT) has been shown to be particularly effective for reducing visceral fat. These short bursts of intense exercise followed by periods of rest can accelerate fat burning, especially in the abdominal area.
Build Muscle with Resistance Training
Incorporating resistance training into your fitness routine is one of the most effective ways to target visceral fat. Building muscle helps to increase your resting metabolic rate (RMR), meaning you burn more calories even when you’re not exercising. Muscles are metabolically active tissue, and the more muscle mass you have, the more energy your body will require to maintain it.
You don’t need to lift heavy weights to see results—bodyweight exercises such as squats, lunges, push-ups, and planks can all help to build strength and muscle. Resistance bands and free weights are also great options. Aim to incorporate resistance training into your weekly routine at least two to three times per week to maximise fat loss.
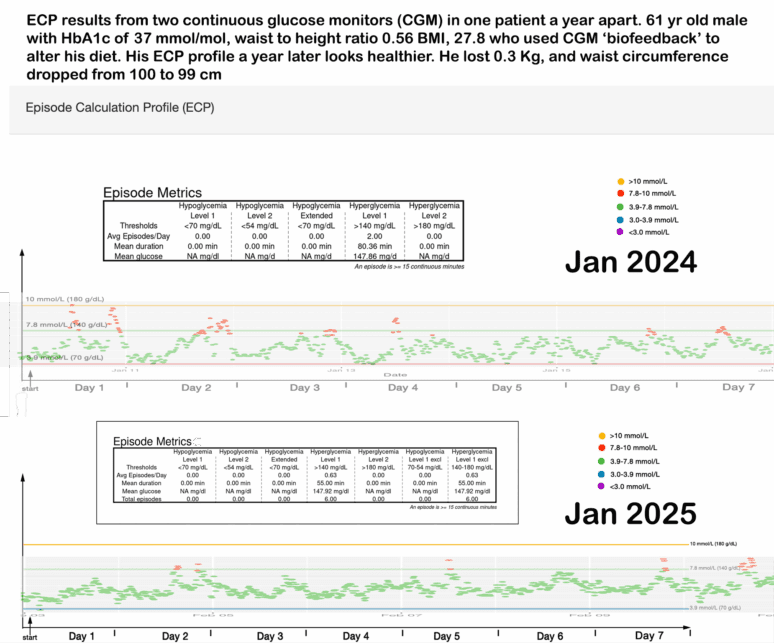
Utilise Continuous Glucose Monitoring (CGM) to Guide Food Choices
Continuous glucose monitoring (CGM) is an excellent tool to guide dietary decisions, particularly for individuals trying to reduce visceral fat. One of the key benefits of using CGM is that it helps identify which foods cause significant glucose spikes. When blood sugar levels rise too quickly, this can lead to an increase in insulin, contributing to fat storage, particularly in the visceral area. By tracking glucose levels in real time, individuals can avoid foods that cause large spikes in blood sugar, such as refined sugars and high-glycemic carbohydrates (e.g., white bread, pastries, and sugary drinks).
The objective of GLP-1 mimetic therapy is often to help regulate blood sugar levels and lower HbA1c, and a CGM can play a crucial role in meeting this goal. By avoiding foods that trigger glucose highs, patients can enhance the effectiveness of GLP-1 treatment and support long-term weight loss. Aim to keep post-meal glucose levels within a normal range, avoiding significant spikes that can contribute to fat storage and insulin resistance.

Track Progress with Body Composition Scales, DEXA and low dose VAT CT scans
Tracking progress is essential—not only to stay motivated but also to ensure your efforts are translating into real metabolic improvements. Traditional bathroom scales measure total weight but tell us nothing about body composition—the balance between muscle, fat, and, most importantly, visceral adipose tissue (VAT).
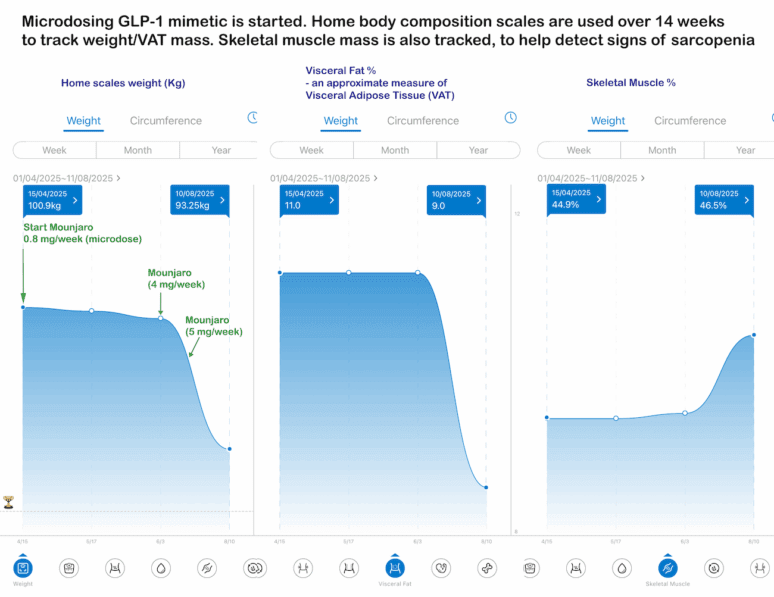
Body composition scales, which estimate fat and muscle mass via bioelectrical impedance, are not as precise as medical imaging, but they can be useful for home monitoring and identifying trends. For example, in the patient case shown below, GLP-1 therapy was started in April 2025 with a gradual weekly dose escalation. Over time, total weight decreased as expected, and estimated visceral fat (via impedance) also fell from 11% to 9%. Importantly, with adequate protein supplementation and a consistent resistance training programme, skeletal muscle percentage actually increased—a key marker of healthy weight loss.
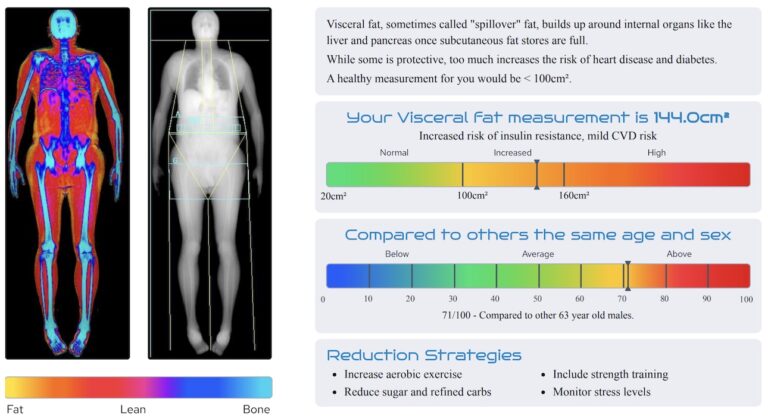
For a more accurate assessment, a DEXA scan can be used. This imaging method confirmed high VAT at baseline for this patient and can be repeated every 6–12 months to track visceral fat reduction, adjust weight goals, and ensure muscle mass is being preserved or increased.
This is particularly important because one of the common pitfalls—both in patients taking GLP-1 mimetics and in those following unsupervised weight loss programmes—is loss of skeletal muscle mass. Without appropriate nutrition and resistance training, this can lead to sarcopenia (age-related muscle loss), which negatively affects strength, function, and long-term health outcomes.


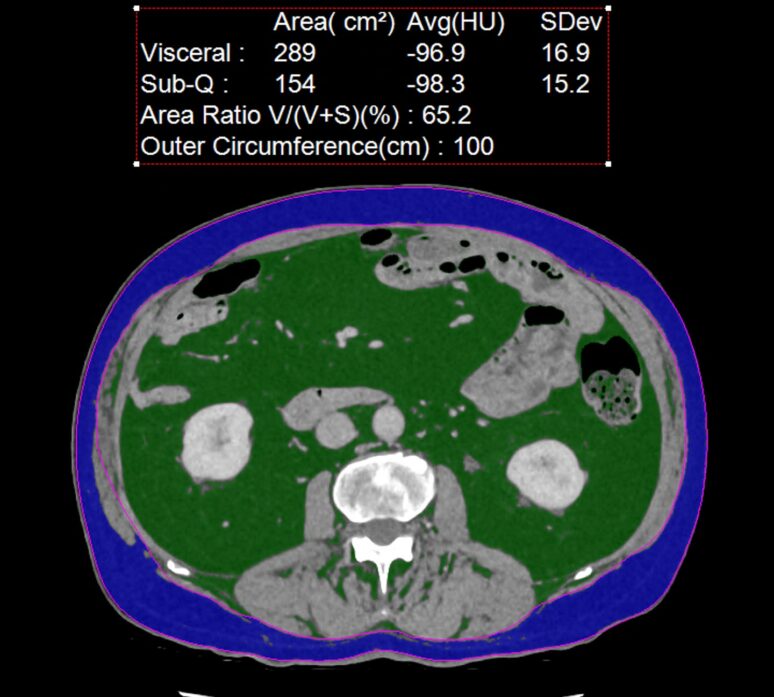
Self refer DEXA scans ( such as shown above) provide a measure of body composition with extremely low dose of radiation, so are ideal for tracking. Low dose CT scans (example below) provide the most accurate direct measure of VAT , but due to higher radiation exposure, require a medical justification.

The figure above illustrates the fat window-processed CT scan of a single slice at lumbar spine level. The back bone is central white, muscle and kidney tissue is in grey while visceral fat is shown in green and subcutaneous fat in blue. A typical threshold value of 100 cm2 is used to define high VAT (as in this case). Low dose abdominal CT slice is the gold standard for an accurate and direct measurement of visceral adipose tissue (VAT). Even though modern CT scan technology can now be used to acquire this information at low doses, the decision to use CT technology needs to be balanced against its risks, therefore must be requested and justified by medically trained health care professionals.
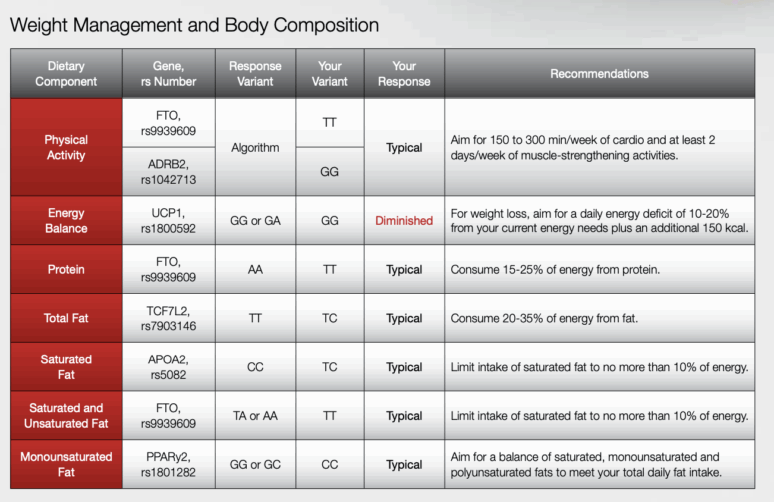
Micronutrients and the Role of DNA Genomics in Targeting Deficiencies
Micronutrients are critical for overall health, and deficiencies in certain vitamins and minerals can have significant effects on metabolism and disease risk. As part of a comprehensive health plan, it’s important to ensure adequate intake of essential micronutrients, including vitamin B12, folate, and vitamin D.
For individuals taking GLP-1 mimetics, such as semaglutide or liraglutide, there may be an increased risk of micronutrient deficiencies, especially in B12 and vitamin D. This is due to the medication’s effects on nutrient absorption, as well as its impact on gut motility. In these cases, DNA genomics can help identify genetic polymorphisms that may predispose individuals to deficiencies in these vital micronutrients.
By using genetic testing and blood work, healthcare providers can identify specific nutrient needs and tailor supplementation strategies for patients taking GLP-1 mimetics. For example, individuals with certain genetic variants might require higher doses of vitamin B12 or vitamin D to support optimal health. Addressing these deficiencies is particularly important for maintaining metabolic health and reducing the risk of complications such as insulin resistance or bone health issues.

In this example taken from a patient’s DNA report provided by Nutrinomix, a genetic polymorphism has been identified that could affect energy balance. Polymorphisms that were possibly once beneficial during prehistoric times of famine may work against us in a time of plentiful food supply.
Conclusion
Losing visceral adipose tissue (VAT) and improving metabolic health is a multifaceted process that requires a combination of dietary changes, exercise, and lifestyle adjustments. For those on GLP-1 mimetics, such as semaglutide (Wegovi) or Tirzepatide (Mounjaro), these strategies can complement the medication’s effects by optimising fat loss, lowering HbA1c, and improving overall health. By utilising tools like CGM, focusing on balanced meals, engaging in regular physical activity, and making smart food choices, you can make meaningful progress in reducing VAT and improving your metabolic health.
These techniques, when combined with personalised strategies such as resistance training, adequate hydration, and mindful alcohol consumption, can help you achieve your weight loss goals and improve your long-term health outcomes. And with the right approach, you may be able to reduce your reliance on GLP-1 mimetics and take control of your metabolic health naturally.
Other related articles
- The Expanding Waistline in Men: Spare Tyre, Killer Visceral Fat, or Just Flabby Abdominal muscles?
- How to Reduce Visceral Fat Without Medication
- GLP-1 mimetic clinic
- Effects of different exercise types on visceral fat in young individuals with obesity aged 6–24 years old: A systematic review and meta-analysis 2022
- Clinical significance of visceral adiposity assessed by computed tomography: A Japanese perspective: 2014
- From Genes to Greens: How DNA Shapes Your Nutritional Needs
- Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement 2019
- Body fat distribution on computed tomography imaging and prostate cancer risk and mortality in the AGES-Reykjavik study 2019