An article written by Dr Edward Leatham, Consultant Cardiologist
Tags: Heart attack, CT angiogram, NH1, search website using Tags to find related stories.
For busy people, or to tune in when on the move, Google Notebook AI audio podcast and an explainer slide show are available for this story beneath.
Coronary heart disease remains one of the world’s leading causes of death. Alarmingly, for over half of those affected, the first symptom is a heart attack—or worse, sudden death.
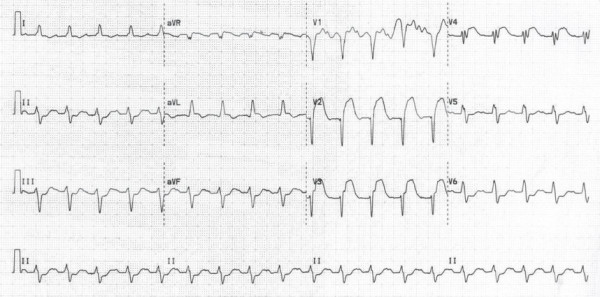
This stark reality underpins why acute coronary syndromes (ACS) are treated with such urgency. The term “ACS” encompasses a spectrum of conditions triggered by a threatened or actual blockage in the coronary arteries. At one extreme is ST-elevation myocardial infarction (STEMI)—a full-blown heart attack requiring immediate intervention. At the other end are non-ST elevation acute coronary syndromes (NSTEACS), which can present with chest pain but without clear ECG changes.
What makes this more complex is that acute coronary syndromes are among the most common reasons for emergency hospital admission worldwide. And yet, paradoxically, the majority of patients presenting with chest pain in the emergency department do not have a coronary cause.
The Complexity of Chest Pain
Why is chest pain so difficult to interpret?
It comes down to the variable innervation of the visceral organs. The sensory nerves serving the heart also overlap with those from the oesophagus and other thoracic structures. This overlap means that problems in other organs can mimic the signs of a heart attack, sometimes perfectly.
Take the oesophagus, for example. It lies in close proximity to the heart and shares a similar sensory nerve supply. When inflamed—due to acid reflux or spasm—it can produce symptoms that are indistinguishable from angina or myocardial infarction. In patients over 30, acid reflux becomes increasingly common, often leading to sensitisation and spasm of the oesophageal smooth muscle, which can generate intense, noxious chest pain.
Musculoskeletal issues also play a role. Entrapment of nerve roots in the cervical or thoracic spine can generate referred pain that mimics the pressure or tightness associated with cardiac ischaemia. Even anxiety and panic attacks can reproduce classical angina-like symptoms, complete with shortness of breath, palpitations and chest tightness.
With so many “mimics”, the real diagnostic challenge lies in deciding which patients are at risk of a serious cardiac event and which can be safely discharged.
The Role and Limits of Troponin
To assist in this critical triage, the medical community turned to a biochemical marker: cardiac troponin.
Troponin is a protein released into the bloodstream when cardiac muscle cells are damaged. In theory, this made it an ideal marker to differentiate true cardiac events from non-cardiac chest pain. Elevated troponin meant myocardial injury. A normal troponin, it might be imagined, means the heart is not the source of the pain or chest symptom.
This ushered in the era of troponin-guided risk stratification. Alongside a clinical assessment and ECG, troponin levels could help emergency physicians decide whether to admit or discharge a patient. The arrival of high-sensitivity troponin assays seemed to improve this further, capable of detecting even microscopic cardiac damage.
But like all diagnostic tools, troponin is not perfect. No test is 100% sensitive and 100% specific, and although very useful for triage (since a raised troponin identifies higher 30 day risk), it cannot reliably detect the presence of a narrowed or severely diseased coronary artery.
The Problem of Troponin-Negative Chest Pain
It is now well recognised that some patients with presenting with warning symptoms due to critical coronary disease and/or dangerous plaque instability may have normal troponin levels, especially in the early stages. In other words, a ‘troponin-negative chest symptoms’ does not always have a benign underlying cause and a normal troponin does not guarantee safety.
Let me illustrate this with a real-world case.
Case Study: The Man in the Car Park
Over a decade ago, I was part of the resuscitation team called to attend a man who had collapsed in the hospital car park. He was found unresponsive and pulseless. The cardiac monitor confirmed ventricular fibrillation, a lethal rhythm disturbance. We delivered an immediate cardioversion—essentially, a controlled electrical shock.
The rhythm was restored, and he was rushed into the emergency department.

His initial ECG showed a classic anterior ST-elevation myocardial infarction—a significant heart attack affecting the front wall of the heart. At that time, primary angioplasty was not yet widely available, so we administered thrombolytic therapy (TNK). Within minutes, the ST elevation resolved, his chest pain settled, and his ECG normalised. He was admitted to the coronary care unit. Over the next 24 hours, multiple troponin measurements and an echocardiogram were performed—all remained within normal limits.
Within 48 hours, we proceeded with an invasive coronary angiogram, which confirmed a critical stenosis (narrowing) of the left anterior descending artery—the so-called “widow-maker” lesion. He underwent a successful angioplasty and made a full recovery.
Now imagine a different scenario: had he not suffered a cardiac arrest, and instead experienced only brief, self-limiting chest pain before arrival, his ECG may have appeared normal, and his troponin levels might never have risen. Under current triage pathways, he may have been discharged from the emergency department with a referral for outpatient investigation.
This case highlights a crucial point: short-lived episodes of cardiac pain caused by threatened coronary occlusion—sufficient to trigger ST elevation and ventricular fibrillation—do not always result in a troponin rise or detectable myocardial injury on echocardiography. As a result, many patients presenting to hospital with the warning symptoms from significant coronary artery disease may be mistakenly triaged as low risk and discharged based solely on normal ECG and troponin findings. The case left a lasting impression on the team and was later published [1].
Since then, however, access to timely investigation through NHS rapid access chest pain (RACP) clinics has become increasingly limited. Because a small but significant proportion of patients with troponin-negative chest pain remain at significant risk all cases should receive outpatient evaluation, ideally within a few weeks, yet current service capacity often fails to deliver this. In some NHS Trusts, RACPC and outpatient waiting times are a great deal longer than 2 weeks, and patients discharged from hospital categorised as ‘low risk’ may therefore wait several months for expert evaluation and diagnostic testing. Tragically, some deteriorate while waiting—there are documented cases of out-of-hospital cardiac arrest and serious complications occurring before formal diagnosis or intervention can be achieved.
The Battle Inside the Artery
This story also underscores a deeper truth about coronary disease.
Within coronary arteries affected by the rupture of an LDL cholesterol laden coronary plaque , a constant biological battle rages between pro-thrombotic forces (designed to seal the breach in the integrity of the arterial wall ) and endogenous fibrinolytic forces (which clear clots to keep blood flowing). When a plaque rupture occurs within a coronary artery—a common trigger for heart attacks—the body responds by activating clotting pathways.
Sometimes, the clot partially forms and then breaks down, restoring flow before permanent damage occurs. This phenomenon—known as spontaneous reperfusion—can result in brief chest pain, no ECG changes, and no measurable troponin rise.
Yet the underlying plaque remains unstable. The patient is still at high risk of a future, possibly fatal, event.
We often refer to these episodes as “stuttering” ACS—periods of transient ischaemia where the artery re-opens spontaneously. Unfortunately, in the absence of ongoing symptoms or troponin elevation, these events are often missed.
The Implications for Care
The implications of this are profound.
While troponin is an excellent tool for rapid triage, it should not be the gatekeeper for further diagnostic testing. A normal troponin level does not rule out serious coronary disease. Clinical judgement must prevail.
That means taking a careful history, assessing the pattern of pain, the timing, the risk factors (such as smoking, diabetes, hypertension, and family history), and not always being falsely reassured by normal blood tests.
In patients where suspicion remains, urgent further testing is warranted—ideally in the form of a diagnostic angiogram. This may be non-invasive (via CT coronary angiography) or invasive, depending on available service capacity and the patient’s risk profile. Other options that can also be helpful albeit with lower predictive value include functional tests such as a stress ECG, stress echo/ MRI or nuclear scan.
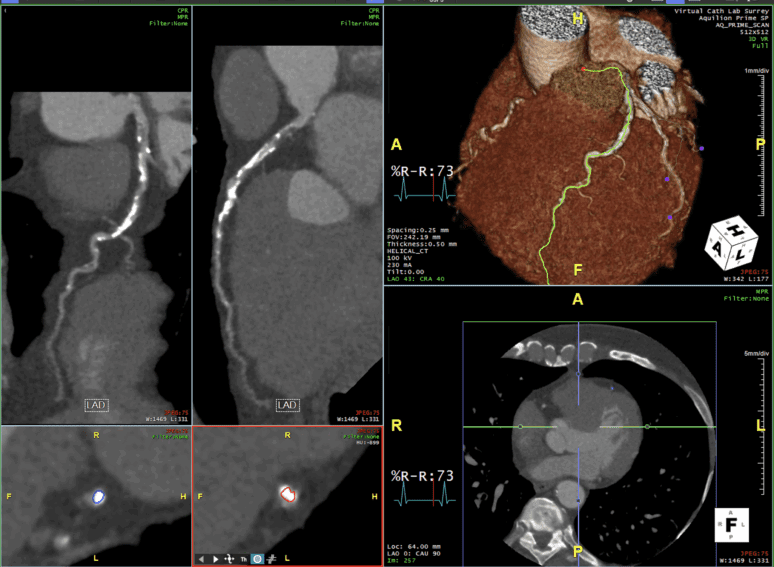
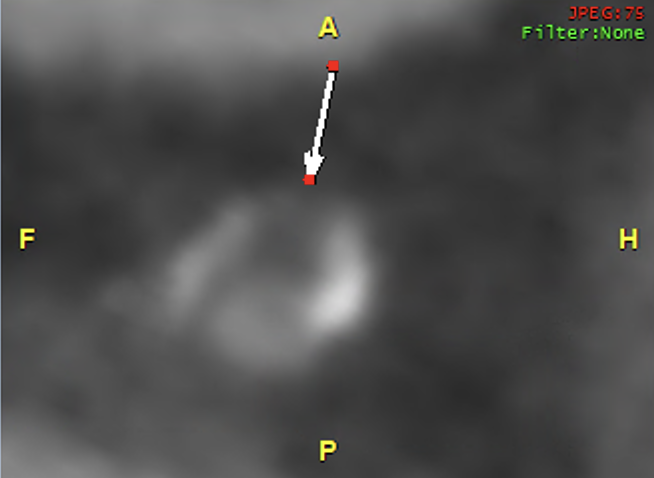
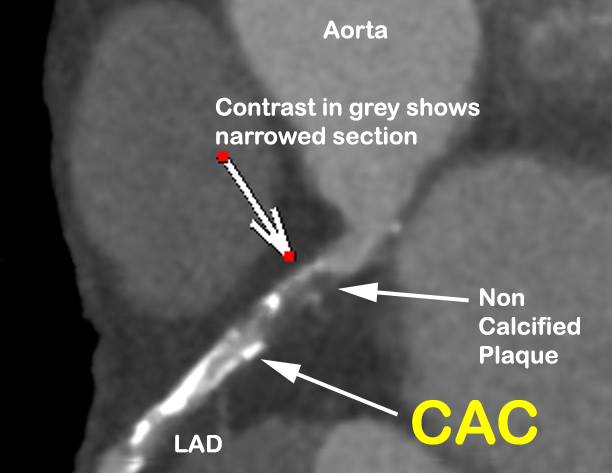
A non invasive CT coronary angiogram

In this overview of a CT coronary angiogram (of a different asymptomatic 62 year old taxi driver attending our screening centre having failed his occupational stress ECG), the course of the left anterior descending (LAD) coronary artery is highlighted in yellow (RH image). There is obvious coronary calcification (bright white) along the length of the LAD. There is a low attenuation ‘dark’ filling defect visible , representing vulnerable non calcified plaque, in the wall of the LAD close to its origin, associated with severe narrowing of the artery. Magnified images of the dangerous plaque (arrows) in longitudinal and a cross section are also shown beneath.. With an anatomic arrangement like this, once a plaque in the proximal LAD disrupts, a platelet initiated thrombus is likely to occlude the LAD, and a heart attack will follow, with characteristic changes, as seen on the ECG above. Early detection of coronary disease on a CT angiogram either on a preventative basis or following some warning symptoms can lead to immediate treatment to prevent a potentially lethal heart attack.


The Bottleneck in the System
Unfortunately, the supply of both invasive coronary angiograms and CT coronary angiography within healthcare systems globally cannot match the demand. While primary angioplasty services have dramatically improved outcomes in patients with STEMI, these are reserved for a small subset of patients. For the rest—those with troponin-positive or non-ST elevation presentations—waiting times for inpatient diagnostic angiography can be 7 to 10 days or longer, even in major hospitals. Troponin-negative presentations are often sent home without a timely work up or prompt imaging tests like a CT angiogram. A delay can be critical. As clinicians, we must identify which patients need further testing urgently. Where clinical suspicion is high, irrespective of troponin rise, doctors and health commissioners should prioritise resources, so that an accurate diagnosis can to be made. Lives literally depend on a prompt anatomic or functional test being done in time. Until these services become widely available, and in good time, patients experiencing unexplained chest symptoms who have not had clinical follow up and diagnosis confirmed are advised to ‘vote with their feet’- either head back into hospital in event of further symptoms, or even consider arranging to fund their own urgent CT angiogram from an independent medical provider.
Key Takeaways for Patients and Clinicians
- Acute or unexplained chest pain or pressure is a red flag. While many causes are benign, some are not. Take all unexplained chest pain/ sensations seriously.
- Troponin is a useful but imperfect tool. A normal result does not guarantee safety, particularly in early presentations or in cases where the chest symptom is fleeting.
- History is everything. Ask the right questions. Listen carefully. A pattern of exertional pain, stuttering symptoms, or radiation to jaw or arms in a patient of the right age (ie over 30) should not be ignored—even if the ECG and troponin are normal. As a guide, if the chest symptoms last less than 15 minutes, a normal Troponin test certainly does NOT rule out high risk ACS.
- Trust your instincts. If something doesn’t feel right, pursue further testing.
- CT coronary angiography is a powerful and tool for assessing both acute and stable patients with suspected coronary disease. It can identify high-risk plaques before an event occurs.
Final Thoughts
In cardiology, we often say that time is muscle. But sometimes, the muscle is lost not in minutes, but in the missed moments when subtle warning signs are dismissed.
Troponin-negative chest pain is one of the most dangerous illusions in modern medicine. As doctors and patients, we must look beyond the numbers and trust the full story.
Because behind a normal troponin, there may lie a plaque waiting to rupture—and a life hanging in the balance.
References
The Naked Heart is an educational project owned and operated by Dr Edward Leatham. It comprises a series of blog articles, videos and reels distributed on Tiktok, Youtube and Instagram aimed to help educate both patients and healthcare professionals about cardiology related issues.
If you would like to receive email notification each week from the Naked Heart, follow me on social media or please feel free to subscribe to the Naked Heart email notifications here